Coronavirus lockdowns may have avoided 531 million infections
Some 60 million may have been avoided in the United States alone

As coronavirus cases began to spike in early 2020, officials in cities around the world shut down parks, stores and more. They also told people to stay home. Two new studies find that the lockdowns were effective at greatly reducing coronavirus infections overall.
Ryan Faas/iStock/Getty Images Plus
As the COVID-19 pandemic developed, some countries imposed “lockdowns.” These included stay-at-home orders for most workers and school children. It also included shutting down all but the most essential businesses. Such measures proved extremely effective. They limited the spread of the new coronavirus. They also saved millions of lives. That’s the conclusion of two new studies.
One of them assessed these impacts in countries hit early: China, South Korea, Iran, Italy, France and the United States. Lockdowns there prevented or delayed an estimated 531 million coronavirus infections, the study concludes. Researchers at the University of California, Berkeley shared their findings June 8 in Nature.
Scientists in England at Imperial College London conducted the second study. It focused on impacts in 11 European countries. Shutdowns there saved about 3.1 million lives. Those interventions brought infection rates down by an average of 81 percent. That is compared to levels before social distancing went into effect. These findings, too, appeared in the June 8 Nature.
R naught — written as R0 — is an estimate of how many other people someone with the virus might infect. In all countries analyzed for the second study, that number was less than one. On average, then, each infected person spread the virus to no more than one other.
That suggests the pandemic would eventually die out if those strict lockdowns had continued.
The new studies suggest “these control measures have worked,” says Alun Lloyd. He’s an epidemiologist who uses math to study the spread of disease. He works at North Carolina State University in Raleigh. He took no part in either study. COVID-19 lockdowns, he concludes, “have saved or delayed many infections and deaths.”
But as countries reopen, a new surge of infections may develop.
Fewer cases
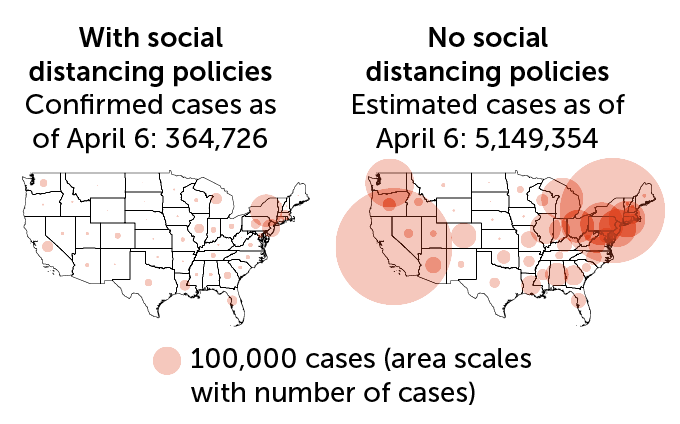
A new study estimates that without social-distancing policies, the coronavirus pandemic’s U.S. impact would have been much worse. How much? An extra 4.8 million confirmed cases by April 6. This analysis comes from researchers at the University of California, Berkeley. It analyzed impacts of stay-at-home orders and business closures. The map at left depicts the reported COVID-19 cases in each state with social distancing in place. The right map shows the estimate of cases if there had been no control measures. The size of the circles indicates case numbers.
U.S. coronavirus cases as of April 6, actual and estimate without social distancing
Worth the trouble, data suggest
COVID-19 cases around the world first began to spike in January, February and March. At that time, China, the United States and Italy enacted tough, temporary measures to slow spread of the virus. These included social distancing and the closure of schools, many stores and restaurants. Many places also restricted all but essential travel.
Such measures disrupted communities across the globe. In many places, a large share of people lost their jobs. With no money coming in, those people have had trouble paying bills. Some even had a hard time buying food. People could no longer meet with friends or family, even for major life events (such as weddings, graduations and funerals). Many people asked whether those changes were worth it: How much did they actually slow the spread of COVID-19?
That’s what the new studies wanted to learn.
“Herd immunity” develops when a large share of the population becomes immune to some disease. Herd immunity can occur when people may already have gotten a disease, recovered and become immune to the disease. It can also happen if enough people have gotten a vaccine that rendered them immune. Among such immune people, a germ now has a hard time finding a new host. How many people must get sick and recover for this to happen depends on how infectious a disease is. And that is defined by the germ’s R0.
Seth Flaxman is an epidemiologist at Imperial College London. When it comes to COVID-19, “We’re very far from herd immunity.” He said that at a June 8 news briefing. In hard-hit places like Italy and Spain, only one in every 20 people have been infected, his team estimates. That’s far from the seven in 10 people that researchers estimate will be needed for herd immunity to this virus.
If people give up the precautions that have protected them thus far, he says, the risk of the pandemic creating a huge new wave of infections “is very real.”
Another way to assess impacts
To gauge how well various virus controls worked, researchers at Berkeley analyzed data in a manner typically used in the field of economics, not health. That method allowed the team to estimate the effect of more than 1,700 local, regional and national policies for the six countries it studied. The team analyzed how fast outbreaks were growing daily. They contrasted the rates before governments had set up virus-control policies to those after.
“Without these policies deployed, we would have lived through a very different April and May,” reports Solomon Hsiang. He’s a data scientist at UC Berkeley. He shared his team’s findings at the June 8 news briefing.
Overall, his group found, lockdowns prevented — or delayed (as the pandemic is not over yet) — some 62 million confirmed COVID-19 cases in the six countries surveyed. Not everyone who gets infected gets tested or even shows symptoms. After accounting for that, Hsiang’s team greatly upped its estimate of the true number of infections avoided. They now think it’s about 530 million people!
That tally covers the time until the lockdowns started being lifted. In the United States, this shows, without lockdowns there could have been 4.8 million more confirmed cases through April and 60 million total infections.
One surprise: Closing schools did not appear to cut the outbreak’s growth, at least in the United States. The data don’t show why. Adding to the problem, Hsiang notes, schools were already closed in some places when the collection of data used in the study began. Who knows how different the results might have been if all schools had been open when the analysis started?
The Imperial College London study used the number of reported COVID-19 deaths from the beginning of the pandemic up to May 4. That’s when Italy and Spain relaxed their lockdowns. By May 4, the study now suggests, up to 15 million people in 11 European countries — including Denmark, Germany, Italy, France and Spain — may have been infected. The team then compared the number of deaths that the analysis predicted without lockdowns to the deaths actually reported. This suggested the lockdowns saved some 3.1 million lives.
Those estimates may be too high, says Julie Swann. She’s a systems engineer at North Carolina State University. The study used a death rate — a measure of deaths per peopled infected — that includes people who never got symptoms. And, she adds, that death rate is at the upper end of current estimates for COVID-19.
This study also assumed that things like school closures or social distancing had the same effect in all countries. No one knows if that’s true. The study’s estimates also assumed people would behave the same way throughout the pandemic. In fact, “people’s behavior changes in response to what they see is going on around them,” Lloyd says. “If things don’t seem bad, people might be less likely to comply [with control measures].” When things are much worse, the opposite may be true.
A host of controls went into effect at about the same time. Which worked best at limiting spread of the virus? Was it social distancing? Shutting down businesses? Limiting long-distance travel? Right now, no one knows.







