Millions of likely U.S. COVID-19 cases have gone undiagnosed
A spike in flu-like illness among untested people may point to coronavirus infections
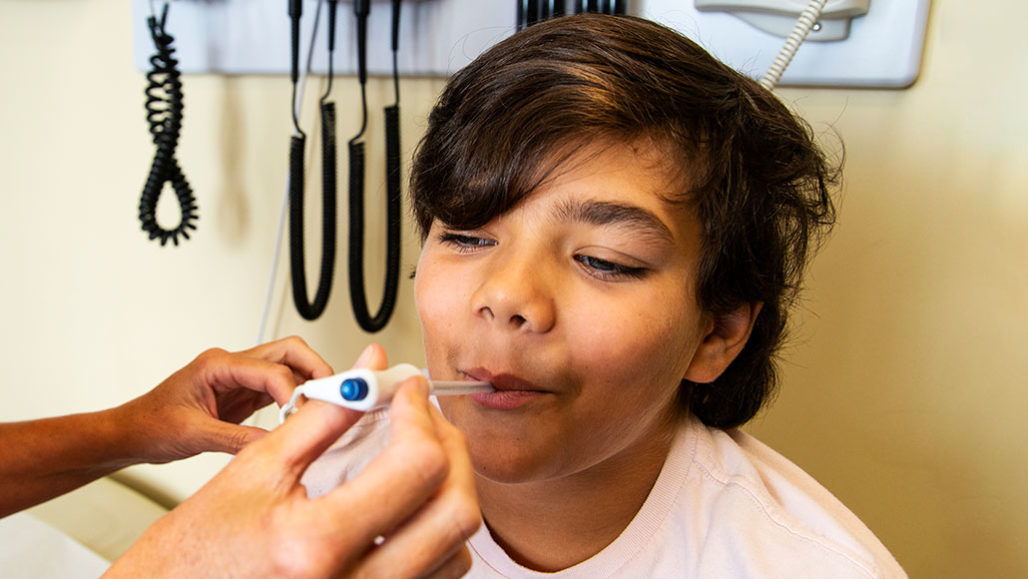
Many people who saw a doctor this past spring with flu-like symptoms didn’t have the flu. Although few of them were tested for COVID-19, a new study concludes that this is likely what millions had.
Fertnig/E+/Getty Images; L. Steenblik Hwang
The COVID-19 virus has now been circulating around the world for more than six months. One never-ending question: How many people has it infected? A new study looking at U.S. data now suggests it may be more than previous tallies had suggested. A lot more.
Officially, there have been more than 2.9 million COVID-19 cases in the United States since January. But that may be a serious undercount, the new study concludes. It projects that more than three times that many people in the U.S. — 8.7 million — may have become infected just between March 8 and 28. If true, more than four in every five of those cases were never diagnosed as COVID-19.
How big an undercount would that be? For perspective, the official global total from December to June 25 was only 700,000 more cases than that three-week U.S. estimate. To date, more than 11.5 million people worldwide are known to have caught the virus.
Any U.S. undercount is likely still ongoing. And if such has happened, U.S. numbers are not likely to be the only ones affected. Issues hiding the identity of most U.S. cases are probably affecting counts of COVID-19 cases elsewhere.
Alex Washburne works at Montana State University in Bozeman. He’s a mathematical epidemiologist. That means he tracks disease by the numbers. In early February, he realized that the number of coronavirus cases was doubling faster than expected. Relatively mild cases, be thought, might be mistaken for something else. To investigate if that might be true, he teamed up with two others. One of them, Justin Silverman, is a doctor and statistician. He works at Penn State University in University Park. The other is Nathaniel Hupert. He’s an internal medicine doctor at Weill Cornell Medicine in New York City.
The three turned to a disease-reporting network run by the Centers for Disease Control and Prevention. It’s called ILINet (for Influenza-like Illness Surveillance Network). Each week, 2,600 doctors send in data collected from nonhospitalized patients throughout the United States, Puerto Rico and the U.S. Virgin Islands.
The cases include people who took a test to see if their infection might actually be flu. Researchers use these numbers to calculate flu rates in the rest of their state or country.
Silverman and his group subtracted cases in the ILINet database where tests had shown these people truly had the flu. This team also subtracted out the expected number of seasonal cases of other flu-like infections. That left them with an apparent large spike in something else.
Data from New York, for instance, turned up twice as many flu-like illnesses that weren’t due to flu than in any March in the past 10 years. (That’s how long ILINet has been tallying such numbers.) The researchers now suspect such extra cases were due to SARS-CoV-2. That’s the virus that causes COVID-19
Washburne, Silverman and Hupert shared what they turned up June 22 in Science Translational Medicine.
Unbelievably high numbers
Their calculations suggested there had been more than 8.7 million COVID-19 cases nationwide. Until that time — March 28 — official numbers had pointed to only some 120,000 confirmed U.S. cases.
“It’s a staggering result,” Silverman says of the excess infections. “I remember calling Alex and saying, ‘This can’t possibly be right. We must have made a mistake.’”
But they checked their math. Before long, Silverman says, “We started believing that this wasn’t just a math error.”
His group assumed that only one in three people infected with the new coronavirus go to the doctor. That’s a reasonable guess, they point out. It’s based on how many people with mild symptoms go to hospital emergency rooms. It also accounts for apparent rates of infections among those who show no symptoms (and, therefore, would not seek out a doctor).
CDC also estimates large undercount of COVID-19
One way to find out if people had recently been infected by a virus is to see if their bodies have made antibodies to it. Such antibody assays in mid-April indicated that close to one-in-eight people who had been tested in New York State had antibodies to the new coronavirus. Governor Andrew Cuomo shared the stat in a news conference on April 23. That number suggests coronavirus infections were already widespread in New York. That number also is in line with the new study’s estimates.
The U.S. Centers for Disease Control and Prevention also has come to suspect a big undercount of COVID-19 infections. CDC Director Robert Redfield fielded questions from the news media in a June 25 call-in by reporters. Redfield said his agency now estimates that for every case that’s been reported, there are actually 10 other infections in the country. This, too, is based on antibody testing.
“It seems possible or likely that ‘surges’ of [flu-like illnesses] may be an indication of a surge in SARS-CoV-2,” says Roger Chou. He’s a doctor of internal medicine at Oregon Health & Science University in Portland.
However, he cautions, the study by Washburne, Silverman and Hupert makes several assumptions. And some of them may not be correct. For instance, Chou says, many cases of excess flu-like illness “are not necessarily SARS-CoV-2.” With everyone scared by COVID-19, he says, these might just be “people seeking care when they wouldn’t in a normal year.”
Another assumption is that the clinics reporting data to ILINet are just like clinics that don’t. In fact, this probably is not the case, says Arthur Reingold. He’s an epidemiologist with the School of Public Health at the University of California, Berkeley. “Can you extrapolate from Santa Clara County [in California] to Montana … or from a study done in the Boston area to Charleston, S.C.?” he asks. “Probably not.”
In the future, Reingold says, direct testing for coronavirus infections is likely to give a better gauge of the size of the ongoing pandemic. This is especially true, he says, since most ILINet clinics report cases only during flu season. That runs mostly from September to early April.







