What kids need to know about getting a COVID-19 shot
A group of new vaccines is rolling out on the speediest schedule in in history

Children and most teens do not yet qualify for coronavirus vaccinations. The vaccines still need to be tested in this age group. But ultimately kids and teens might be asked for proof of such a vaccination to play team sports.
Pollyana Ventura/iStock/Getty Images
On December 14, the first Americans got a vaccine designed to protect them from COVID-19. Health-care workers were put at the head of the line to get these shots. So were older adults living in care facilities. That’s according to guidelines from the Centers for Disease Control and Prevention, or CDC. Over the coming months, other groups of adults will qualify for vaccination. But kids under age 16? They won’t be getting the shots. At least not yet. However, plenty of doctors are anxious to see that change.
There are many coronavirus vaccines being developed. Three big drug companies — Pfizer, Moderna and AstraZeneca — have all reported results that their vaccines could be at least 90 percent effective in fighting the virus. The Pfizer and Moderna vaccines received emergency approval from the U.S. Food and Drug Administration (FDA) last month. They are now being given to some adults.

Yet none of these vaccines are ready for kids. Pfizer is studying its vaccine in children over age 12. But that effort began only a few months ago. Moderna will start testing its vaccine on kids early this year. The delay in testing kids means it could be many months before the FDA approves vaccinations for anyone under 16.
There’s never before been a vaccine for COVID-19, and there is much to learn about these new ones. Rarely has a vaccine been created in less than a decade, much less in a matter of months. So for the new, fast-tracked vaccines, it’s good to ask questions about safety. A COVID-19 vaccine could save thousands of lives every week, says Preeti Malani. She’s a doctor of infectious diseases at the University of Michigan in Ann Arbor.
And because COVID-19 affects kids and adults differently, it’s important to understand whether a vaccine might work equally well in everyone. Kids will play a key role in ending the pandemic, but they won’t be able to get the vaccine until experts verify it’s safe and effective for that age group.
Dealing with the coronavirus emergency
Scientists usually make vaccines in a linear process: They take one step first, then the next and so on. But the COVID-19 pandemic has accelerated things. Tens of millions of people worldwide have been infected. More than 1.8 million have died. Governments have asked scientists to move faster.
And scientists stepped up. They started with the vaccine design process. Fortunately, they were able to use new technology that has worked for other similar types of viruses. As a result, they were able to start clinical trials in record time. In these trials, the vaccine is tested in increasingly large groups of people to see if it’s safe and effective.
The human trials are employing the best type of research, says Robert M. Jacobson. He’s a pediatrician and vaccine researcher. He works at the Mayo Clinic Children’s Center in Rochester, Minn. In these trials, adults of all ages are randomly assigned to get either the real vaccine or a placebo (a fake, inactive shot). No one knows until the trial is over who got the real medicine and who didn’t. These are known as randomized, controlled clinical trials with placebos.
After a vaccine has been shown to be safe and effective in clinical trials, there are still more steps before it can be given to everyone. This includes being reviewed and approved by a government agency. In the United States, the FDA is in charge of vaccines and other drugs. It can speed a vaccine’s development by giving drug makers something called an emergency use authorization.
Vaccines can’t get this “just because manufacturers want it,” Malani points out. And getting it “doesn’t mean the full review process is not going to happen,” she adds. “It just means we can speed [that process] along.” The speed comes from letting drug companies work on multiple steps at the same time.
“It’s not sequentially, but simultaneously,” explains Jill Weatherhead. She’s a doctor at Baylor College of Medicine in Houston, Texas. There, she specializes in pediatric infectious diseases.
Companies can further speed up the process by starting manufacture of the vaccine before the trials are even over, Weatherhead notes. That may cut months to a year from a vaccine’s initial roll-out. Also, some COVID-19 vaccines, she points out, use new technology that allows manufacturers to make lots of them more quickly than is possible with older technologies.
The FDA has convened many meetings on these vaccines to speed things up. Governments and manufacturers also have spent billions more dollars than usual, which helps things go faster.
All of this means that scientists have been able to create vaccines quickly without sacrificing safety, says Jacobson. “Using the latest science,” he says, has dramatically sped up the vaccines’ development. And, he adds, “There’s no evidence that indicates [the companies] are cutting corners.”
One thing scientists can’t speed up is time. Before presenting results to the FDA, the researchers needed at least two months of data. That let them see whether the vaccines were effective in keeping people from getting sick, and whether the participants experienced any major side effects. Those usually show up in the first two months. But experts won’t know right away if there are any long-term side-effects from a vaccine. And they can’t say how long its protection will last. So studies will keep tracking vaccinated people for years. That’s not unusual. Even under normal circumstances, Jacobson points out, such long-term impacts aren’t known before a new vaccine is given to the public.
“We need the vaccine as soon as it is safe and effective — but not any sooner,” Jacobson says.

Why do kids have to wait?
Health-care workers are getting the first doses of approved vaccines. Elderly people in care homes are next on the list. Then comes other groups of adults. Where does that leave kids?
“They’re not high on the list for a number of reasons,” notes Jacobson. States will give highest priority to people at highest risk of getting very sick or dying from the virus. They will also give priority to people most likely to be exposed, such as health-care workers and essential workers (this last category includes grocery and transportation workers). In some states, teachers are high on the list.
Unlike adults, most kids who become infected with the new coronavirus get mild disease. A few may get seriously ill, including some athletes. And students may spread the disease to parents or teachers or grandparents. Eventually, children and teens will need to be vaccinated. In fact, argues Jacobson, “We’re not going to be able to control the pandemic until children are vaccinated.”
But before that can happen, scientists need to study how the vaccine works in children. The American Academy of Pediatrics demanded in November that research begin involving more kids, and “very soon.”
“More than one million children have been infected with this virus since the beginning of the pandemic,” notes the academy’s president Sally Goza, a doctor. And even those who did not get severely ill have suffered in many ways. Their education has been disrupted. Many now experience stress and mental-health problems. Moreover, doctors overworked with caring for critically ill COVID-19 cases have little time to handle the medical needs of others, including sick children.
As such, Goza argues, “It is unjust to allow [kids] to take on these burdens but not give them the opportunity to benefit from a vaccine.”
One big problem: The vaccine trials initially didn’t include kids.
“The rule is you don’t give a vaccine in an age group you haven’t studied,” Jacobson explains. What’s more, he adds, pediatric research requires “a higher bar of safety.” A new treatment must be shown at least as safe for children as it is for adults.
Work with other vaccines has shown that these drugs do not tend to work the same for all age groups.
The flu vaccine, he notes, doesn’t work in babies under 6 months old. The measles, mumps and rubella vaccine doesn’t work in babies under a year old. And kids under age 9 need two doses of the flu vaccine each year, not one. Older kids, in contrast, need more doses of the HPV vaccine than younger adolescents. “So age plays a huge role,” he says.
Children older than about 8 years old also have the right to refuse to participate in a vaccine trial, Jacobson notes, even if their parents want them to.
How safe are vaccines?

Simply put, “vaccines are the safest medicine ever developed,” Jacobson says. “Vaccines are far safer than prescription or non-prescription medications, vitamins, minerals or food supplements.”
What’s more, he adds, “vaccines are far safer than the antibiotics I prescribe, the high-blood-pressure medicines adults often take, the acetaminophen and ibuprofen we all take for aches and pains.”
The standards for vaccine safety have to be higher, he points out. People will sometimes accept some risk from a medicine because of the tradeoff that it will help treat some problem they have, such pain or an illness. In contrast, vaccines go to people who are well. You don’t want to risk making a healthy person sick.
That does not mean, however, that there are never side effects. Some people in the COVID-19 vaccine trials developed fever or chills after getting their shots. That’s actually a sign that their immune symptom is kicking in and that the vaccine is doing its job. Some people also have experienced temporary swelling where the needle went in. And a handful of people experienced a bad allergic reaction after being vaccinated.
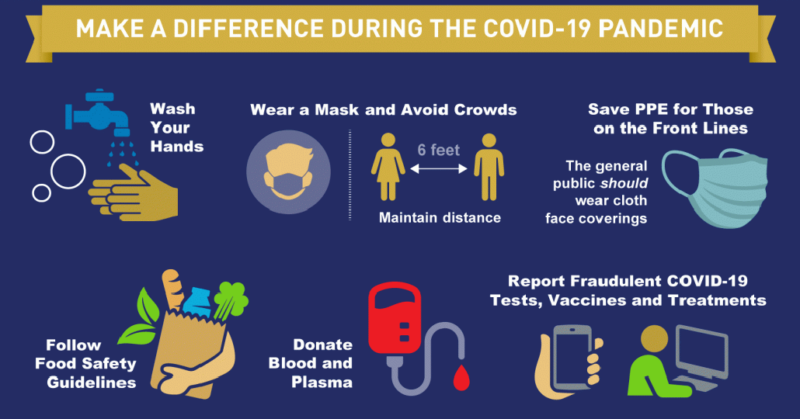
Someday, a COVID-19 vaccine may be required to go to schools, to sporting events, to visit nursing homes — even to travel or to play sports. But until most of us get vaccines and we reach herd immunity, we’ll all still have to wear masks, wash our hands a lot and stay a safe distance away from friends. (Herd immunity is when enough people in a community have become immune to an infectious disease that germs have a hard time finding a new victim. When this happens, a disease tends to die out naturally.)
“Kids don’t always get credit for what they’ve given up,” says Weatherhead at Baylor. “It’s important to recognize their effort and role in protecting the community” by continuing to wear a mask, keeping a physical distance from others and washing their hands. The good news: “It’s going to pay off in the long run,” she says. “And the end is hopefully on the horizon. Scientists are working around the clock so [that kids] can get back to being teenagers.”







