Explainer: What is sickle cell disease?
C-shaped blood cells can get caught in vessels, causing pain and worse

In the right circle is an illustration of the sticky, sickle — C-shaped — form that red blood cells can develop when the hemoglobin inside them has stacked together. A normal red blood cell is on the left. A gene mutation underlies this sickling, a hallmark of painful sickle cell disease.
wildpixel/iStock/Getty Images Plus
By Erin Garcia de Jesús and Janet Raloff
Our genes serve as an operating manual for cells of the body. Genes tell cells what to do and when. But copying errors in those operating manuals — known as mutations — can lead to misspelled instructions that can change how cells operate. Scientists now know that some of those mutations can lead to disease. Others offer benefits. Some can do both. And the mutation that underlies sickle cell disease is one that can be both good and very bad.
Sickle cell disease is caused by a molecular change in the body’s hemoglobin.
Hemoglobin is the molecule in red blood cells that transports oxygen to tissues throughout the body. It wasn’t until 1949 that scientists learned altered hemoglobin causes red blood cells to take the shape of crescent moons. In fact, this condition was the first known example of a disease linked to inherited changes in a molecule.
Hemoglobin normally allows “red blood cells to be very floppy and pliable, and slip and slide through the blood vessels easily,” says Erica Esrick. She’s a pediatrician at Boston Children’s Hospital and Harvard Medical School. Both are in Boston, Mass.
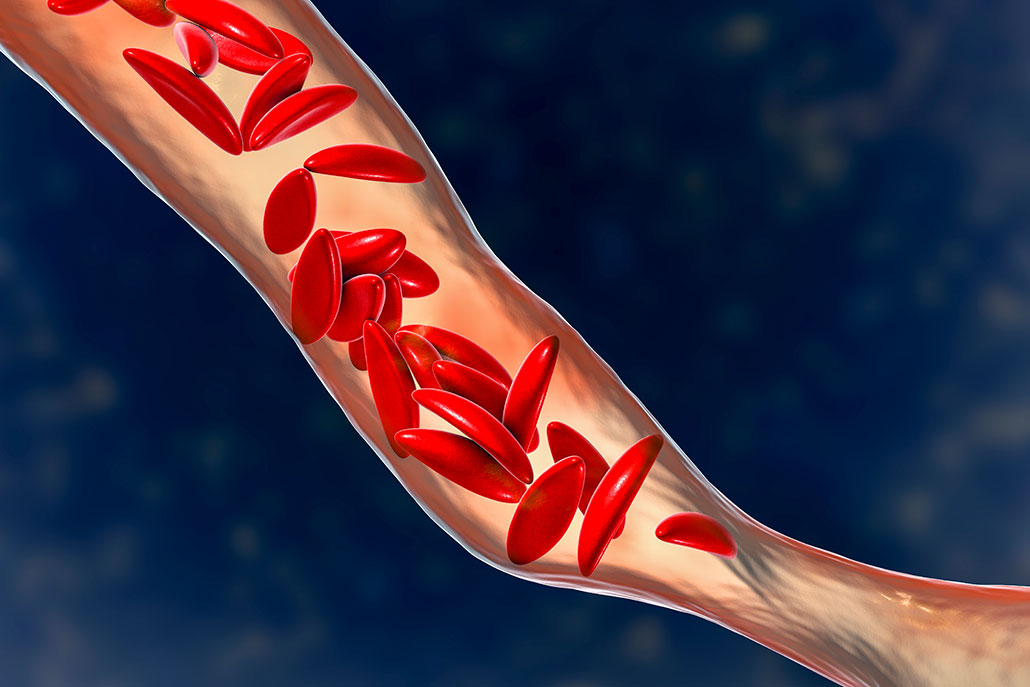
But a mutation in a single hemoglobin-making gene — the HBB gene — underlies sickle cell disease. This mutation makes hemoglobin stack in long strings inside blood cells. It gives those cells an inflexible, sickle — or crescent-moon — shape. Instead of being “squishy,” the now-stiff red blood cells get stuck inside blood vessels. This can cause severe and debilitating pain. Worse still, the sickle cells can literally block blood flow and the movement of oxygen into nearby tissues.
Most people with sickle cell disease live only into their late 40s. Among other reasons, the blocked blood vessels that this disease often causes can lead to strokes or organ damage.
To develop this disease, people must inherit that mutant HBB gene from both parents. If they get the mutant from one parent only, their blood cells can work normally.
Sickle cell affects millions of people around the world. In the United States, for instance, about 100,000 people live with the disease. Most of them are Black or Latino. The mutation behind it is particularly common in people whose ancestors came from parts of Africa that are south of the Sahara, from parts of the Middle East or from Southeast Asia. Why? It turns out that these areas have high rates of malaria.
Malaria afflicts an estimated 241 million people. In 2020 alone, it killed an estimated 627,000 people, according to the World Health Organization. And the mutant HBB gene makes the body resistant to infection by the parasite that causes malaria. Once the mutant gene first emerged, it spread widely in parts of the world where it conferred this resistance to malaria. But that benefit is overshadowed when someone inherits the mutant gene from both parents and develops sickle cell disease.
A bone marrow transplant is currently the only cure for sickle cell disease. A new marrow can make unsickled red blood cells. But such transplants are costly. Finding a matched donor to contribute marrow also is challenging, Esrick notes. That’s one reason researchers have begun looking to replace the mutant HBB genes. Esrick is part of one research team that is currently trying to fight the disease through such gene therapy.







