A ‘mini cyclone’ helps detect coronavirus in the air
In just five minutes, the tabletop device can identify trace amounts of COVID-19 virus
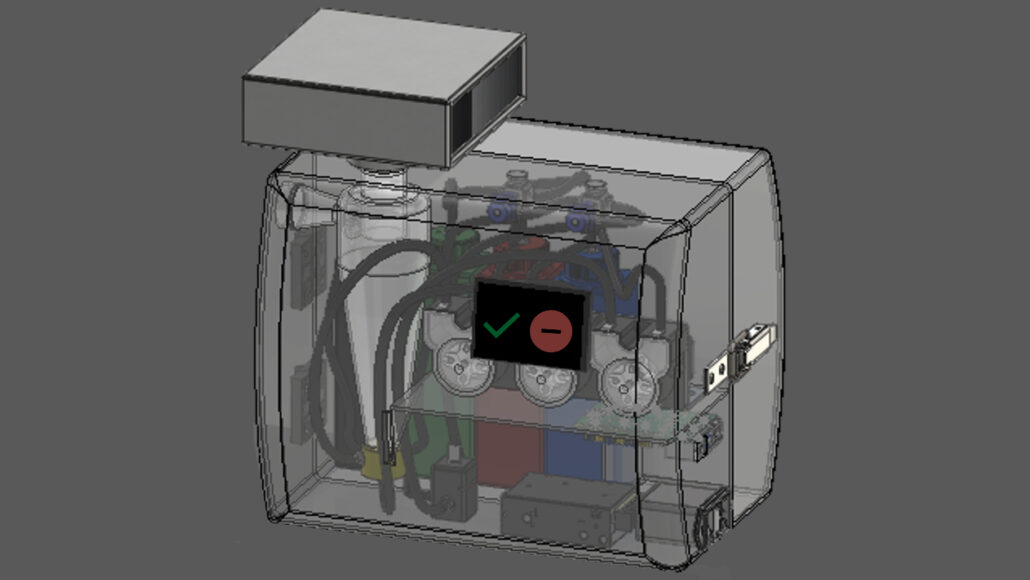
Scientists have created an air-sampling machine that takes just minutes to detect the virus that causes COVID-19. This 3-D illustration shows the proposed final design of that device.
Joseph Puthussery/Washington Univ. in St. Louis
If you ever walk into a room and wonder if the virus that causes COVID-19 is hanging around, you’re not alone. Now there’s a device that could answer that question. Researchers have created an air-sucking machine able to quickly detect the coronavirus.
The machine is a little bigger than a toaster. In just five minutes, it can detect as few as seven to 35 particles of the SARS-CoV-2 virus per cubic meter (35 cubic feet) of air. That’s about the same sensitivity as nasal swab tests that rely on PCR, says Rajan Chakrabarty. He’s an aerosol scientist at Washington University in St. Louis, Mo.
His team described its innovation July 10 in Nature Communications.
One challenge the team faced was collecting enough air to concentrate the coronavirus particles. Earlier systems developed by others sucked in between two and eight liters (quarts) of air per minute. This sampler pulls in 1,000 liters each minute.
To trap the virus, Chakrabarty says, his team created “an artificial cyclone inside of the sampler.” Once inside, the air is mixed with liquid in a fast-paced swirl. This cyclonic action slings the slurry against the detector’s wall. Any viruses will now concentrate there.

Educators and Parents, Sign Up for The Cheat Sheet
Weekly updates to help you use Science News Explores in the learning environment
Thank you for signing up!
There was a problem signing you up.
A HEPA filter attached to the device removes any airborne viruses not captured in the liquid. After five minutes of collection, the system pumps the virus-rich liquid to a biosensor.
That sensor has an electrode attached to a specialized immune-system protein made by llamas and their relatives. Known as a nanobody, it fights infections like human antibodies do. But this protein is smaller and somewhat tougher.
The nanobody grabs the spike protein on any passing coronavirus. Electricity flows from the electrode through the nanobody and spike protein. That causes a particular amino acid — a building block of the spike protein — to lose electrons. Their loss causes a change in voltage. And that signals that SARS-CoV-2 is present.
Real-time detection
The Washington University team placed its device in the apartments of two volunteers. Each had a confirmed COVID-19 infection. This would allow the team to test how well the tool could detect the virus in real-world conditions.

And it detected “even the trace amounts of virus being shed by the patients,” Chakrabarty says. When placed in an empty, well-ventilated conference room, the device turned up no virus.
“They’ve demonstrated that it works,” says Linsey Marr. She’s an aerosol scientist at Virginia Tech in Blacksburg. This new system can “detect [the] virus at low levels that we would be concerned about in the air,” she says. As part of studying how germs spread, Marr’s team is also developing a virus detector.
Some challenges remain. For one, the new device is noisy — about as loud as a vacuum cleaner or a ringing phone. People might find that tolerable for a short run. But that’s too loud, Marr says, to run non-stop in a classroom or office.
The system is costly, too. Chakrabarty says the cost of building one in a research lab runs around $1,400 to $1,900.
Commercial versions may start out too pricey for home use, Marr says. But she thinks hospitals, airports and other public areas could benefit from them. It might be possible to link the devices into the air supply for systems that heat, cool and ventilate buildings. Those systems could then ramp up air flow and filtration when virus is detected.
Meanwhile, Chakrabarty is already thinking of next steps for his team’s device. He hopes to add llama nanobodies to detect other airborne viruses as well, such as the one that causes flu.