Behavior of genes could identify type of infection
Distinguishing viral from bacterial infections could guide treatment
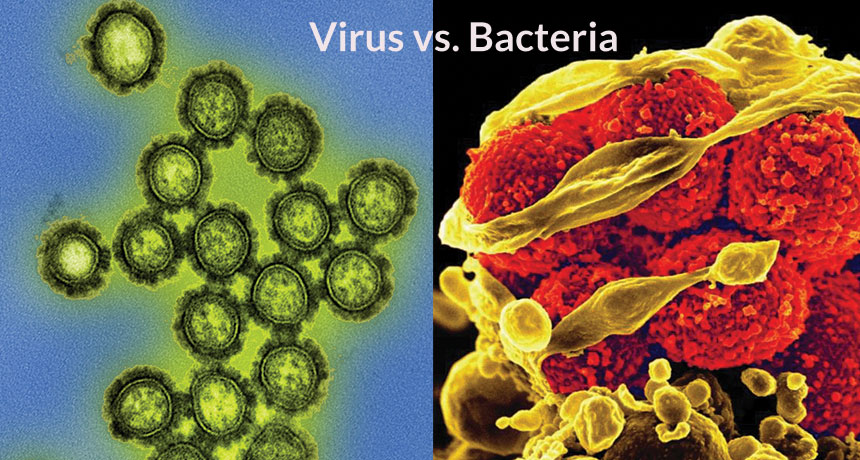
How certain genes behave in sick people can reveal whether an infection was caused by a virus, such as the H1N1 influenza virus (left), or by bacteria, such as methicillin-resistant Staphylococcus aureus, or MRSA (right).
NIAID/FLICKR (CC BY 2.0)
Coughs, fevers and green mucus can accompany a respiratory infection. Most of the time, doctors can only guess whether bacteria or viruses were responsible. A new study now points out a new way to identify the perp.
An infection changes the actions of the sick person’s genes. And that response differs depending on whether bacteria or viruses are doing the damage, scientists now report. Knowing which it is could help doctors quickly figure out what ails a person. And it could tell them whether the best treatment is antibiotics, antiviral drugs or just chicken soup and sleep.
The researchers found a telltale sign, or signature, in genes when people were infected by a virus. That started them combing through datasets that included information about how human genes behave after an infection. The team looked at three types of viral infections. The first was influenza, or flu. The second was the common cold, caused by the human rhinovirus. The third was respiratory syncytial virus, or RSV. RSV causes symptoms similar to the common cold in most people. Babies and older adults, however, can develop more serious conditions, such as pneumonia.
Using clever mathematical analyses, the researchers combed through the datasets. Out of this search popped one consistent calling card for viral infections. This was a set of nearly 400 genes. Each grew either more or less active during a viral attack. Not surprisingly, many of the genes tell the body to make proteins involved in inflammation and other responses to viruses.
The team then tested whether these genes had behaved differently from when a person had a bacterial infection or no infection at all. This time, the researchers looked at different datasets that weren’t used to make the gene list. The virus signature could predict whether a person was infected with a virus, they found. The gene response was very strong, says Purvesh Khatri. He is an immunologist at Stanford University who led the new study. That signature didn’t show up in bacterial infections or in healthy people. Khatri’s team described its new findings in the December 15 Immunity.
Viral signatures are very distinct
The newfound gene changes are “the most solid signature people have found,” says Shai Shen-Orr. He is an immunologist at Technion-Israel Institute of Technology in Haifa. He was not involved with the new research. Because the viral signature was consistent across many studies, the results have added strength. “It’s like this has just been lying here, waiting for someone to pick up,” he says. “The signal just jumped out.”

Khatri’s team gathered data from studies in which healthy people were infected with flu. And the viral signature showed up hours before symptoms appeared. The method even identified people who were infected but didn’t feel ill. “We could pick up a person walking around, not showing any symptoms,” Khatri says.
The analysis also offers clues about how well a flu vaccine has worked. The body’s response to flu shots was similar to what occurs during an actual bout of flu. The behavior of the 11 genes reliably changed in both cases, the new research showed. That result should one day let doctors track how well a flu shot worked.
Khatri and his team turned up a curious difference between men and women. Gene responses to flu peaked the first day after a man got his flu shot. In women, those changes took three days to peak. Some studies have waited several days to look for a response to flu shots. And they tended to conclude that men respond more weakly, Khatri says. But it now appears that a man’s earlier responses simply may have been missed by such studies.
The strength of the new work comes from its use of many diverse datasets, says John Tsang. He is an immunologist at the National Institute of Allergy and Infectious Diseases in Bethesda, Md. “The key here is that after you look across all of [the datasets], you see a coherent signal,” he says. “That’s the encouraging sign.”
Tsang, who was not involved in the study, warns that before this new virus-detection system would be useful, it first must be tested in a large study. It would have to be able to detect changes over time in how genes behave.
Khatri and his colleagues are already working to design a test that could tell doctors whether a patient has a viral or bacterial infection. Such a test would cut down on unnecessary antibiotic use, Khatri says. The reason: Those drugs do not fight viruses. So doctors would only prescribe these drugs to rout bacteria.
Power Words
(for more about Power Words, click here)
antibiotic A germ-killing substance prescribed as a medicine (or sometimes as a feed additive to promote the growth of livestock). It does not work against viruses.
antiviral A virus-killing substance prescribed as a medicine.
bacterium (plural bacteria) A single-celled organism. These dwell nearly everywhere on Earth, from the bottom of the sea to inside animals.
dataset (or data set) A large, discrete group of data collected or assembled for a particular purpose.
gene (adj. genetic) A segment of DNA that codes, or holds instructions, for producing a protein. Offspring inherit genes from their parents. Genes influence how an organism looks and behaves.
immune Able to ward off a particular infection. Alternatively, this term can mean to show no impacts from a particular poison or process. More generally, the term may signal that something cannot be hurt by a particular drug, disease or chemical.
immunology The field of biomedicine that deals with the immune system. A doctor or scientist who works in that field is known as an immunologist.
infection A disease that can spread from one organism to another.
inflammation The body’s response to cellular injury and obesity; it often involves swelling, redness, heat and pain. It is also an underlying feature responsible for the development and aggravation of many diseases, especially heart disease and diabetes.
influenza (or flu) A highly contagious viral infection of the respiratory passages causing fever and severe aching. It often occurs as an epidemic.
mucus A slimy substance produced in the lungs, nose, digestive system and other parts of the body to protect against infection. Mucus is made mainly of water but also includes salt and proteins such as mucins. Some animals use mucus for other purposes, such as to move across the ground or to defend themselves against predators.
pneumonia A lung disease in which infection by a virus or bacterium causes inflammation and tissue damage. Sometimes the lungs fill with fluid or mucus. Symptoms include fever, chills, cough and trouble breathing.
respiratory Of or referring to parts of the body involved in breathing (called the respiratory system). It includes large airways, such as those in the nose, throat, sinuses and lungs.
respiratory syncytial virus (RSV) A virus that infects the lung and respiratory passages in humans. In most people, it causes symptoms similar to the common cold. Symptoms can be more dangerous in infants and older adults.
rhinovirus One of the most common viruses that causes the common cold.
vaccine A biological mixture that resembles a disease-causing agent. It is given to help the body create immunity to a particular disease. The injections used to administer most vaccines are known as vaccinations.
virus Tiny infectious particles consisting of RNA or DNA surrounded by protein. Viruses can reproduce only by injecting their genetic material into the cells of living creatures. Although scientists frequently refer to viruses as live or dead, in fact no virus is truly alive. It doesn’t eat like animals do, or make its own food the way plants do. It must hijack the cellular machinery of a living cell in order to survive.







