Decades-long project is linking our health to the environment
Findings come from tracking health and habits in three generations of California families

By studying three generations of California families, scientists are gaining valuable clues about the role of the environment on health.
kate_sept2004/iStock/Getty Images Plus
Share this:
- Share via email (Opens in new window) Email
- Click to share on Facebook (Opens in new window) Facebook
- Click to share on X (Opens in new window) X
- Click to share on Pinterest (Opens in new window) Pinterest
- Click to share on Reddit (Opens in new window) Reddit
- Share to Google Classroom (Opens in new window) Google Classroom
- Click to print (Opens in new window) Print
Isabel Katz was 14 when she found out her mom and grandma were part of a long-running science program. “I was really surprised,” she says. Started in 1959, it’s one of the oldest ongoing research programs in the world. It has collected data on thousands of families like Isabel’s that live in and around San Francisco, Calif.
The program is known as the Child Health and Development Studies, or CHDS. Over the decades, its researchers have shared many of their findings at meetings and in journals. Each of these reports can be thought of as one of the “studies” in CHDS. But it in terms of research, it makes sense to just think of CHDS as one super-long-running study with many parts.
Scientists have learned important things from the families taking part. In the 1960s, for instance, researchers showed that women who smoked during pregnancy tended to have smaller babies. This led other researchers to study how a mom’s smoking can harm her unborn baby.
This massive study is now giving scientists other important clues about what roles the environment plays in human health. “What makes this study rare is that it spans three generations,” notes lead scientist Barbara Cohn. This and other long-running studies like it might one day help people make changes to the environment in ways that can reduce how many people get sick.
Understanding environmental risk
Before such changes can happen, however, we need to know what to change. Many diseases have more than one cause. Several factors determine who gets conditions such as autism, celiac disease, diabetes and cancer.
Genes are fragments of DNA that determine how an organism looks and acts. We inherit genes from our parents. Those genes also help determine who may develop certain diseases. Certain behaviors — such as how much we exercise or sleep — also play a role.
So can influences over which we have less control, such as what’s in the food we eat, the water we drink and the air we breathe. These environmental factors can include our exposures to harmful chemicals. These can enter our bodies through the skin, lungs, nose or gut.
Some examples of potentially risky chemicals include bisphenol A (BPA), an ingredient of plastics, dental sealants and the inks in some thermal-printing papers. Another big class of such compounds are perfluorinated chemicals. These “nonstick” agents are used to coat many frying pans, food packaging materials and fabrics. There are also potentially toxic pesticides and pollutants spewed by the burning of everything from fossil fuels to drought-stricken forests. Even the natural ingredients in foods can sometimes affect our risk of disease.
We can’t easily change our genetic makeup. But we might be able to change some aspects of the environment to which we will be exposed. First, however, there’s a lot more research that needs to be done. “We don’t know what those important environmental factors are for a lot of diseases,” notes Brandon Pearson. He’s a neuroscientist at Columbia University in New York City. His work focuses on impacts of toxic chemicals on the brain.
Understanding those environmental risks, Pearson point out, starts with observation.
Learning from the past
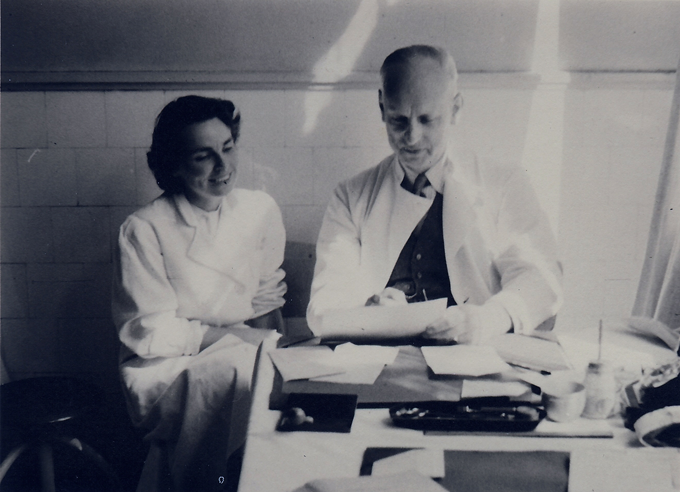
Barbara Cohn spends much of her day at a computer, not a lab bench. Her Berkeley, Calif., office contains an electronic portal to the past. She is the keeper of health information spanning three generations.
Cohn is an epidemiologist. Such researchers study large groups of people. They’re known as cohorts. To study a cohort’s health over time, researchers often take blood samples, ask questions and collect other data. They may do this every few months or every few years. Then they track how, on average, the health of the recruits have changed over time.
Scientists use these data to identify patterns of disease. They also can look for any details on what might have boosted — or lowered — the chance that people in the cohort developed a particular disease.
This is called observational science. Researchers can use it to generate a new hypothesis (Hy-PAH-thuh-sis). Hypotheses are sort of educated guesses that are based on one or more observations.
For example, during World War II, researchers saw the first clues that a baby’s environment in the womb might help predict who, in adulthood, would go on to develop certain diseases. In the winter of 1944 to 1945, the Nazis had taken over the Netherlands. This caused a severe famine. Adults in many parts of the country lived on just 400 calories a day. (A normal adult diet is closer to 2,000 calories a day.) Babies born during this so-called Dutch “Hunger Winter” famine were shorter and thinner than babies born before or after.
But even years later, people born during the famine were more likely to suffer from diseases such as heart disease and diabetes than were their peers born shortly before or after them. Researchers hypothesized that a mother’s starvation during pregnancy changed how her baby developed in the womb. These changes made the famine babies more vulnerable to certain diseases.
These data also show that it can take many years after an exposure for symptoms of disease risk to emerge. And that can make it difficult to identify links between the environment and health. Long-running cohort studies are one of the best tools scientists have for finding such links, Cohn says. That’s because cohort studies allow scientists to collect health data from the same people throughout their lives.
Families volunteer
Isabel Katz’s grandmother, Ruth Deuel, joined the Child Health and Development Studies in 1962. It was a few days after Deuel had given birth to Isabel’s mom, Jennifer Iscol. A nurse at the hospital asked Deuel if she wanted to volunteer for a science study. It would look for patterns between the health of mothers during pregnancy and how their babies grew over time. As a computer programmer, Deuel had a strong interest in science. She thought, “Sure, why not?”
Deuel answered questions about her health and habits. Did she smoke? Had she taken any medicines during her pregnancy? Nurses measured her height, weight and blood pressure. They collected a vial of her blood. They also collected data from her daughter, Jennifer, as she grew from an infant into a child.
From these data, the researchers learned many things. For instance, mothers who smoked during pregnancy gave birth to smaller babies. Babies born too small can develop breathing problems and other health issues. Other studies also showed that smoking during pregnancy might harm growing babies. So doctors began advising pregnant women not to smoke.
Scientists continued to collect data as Jennifer and other children in her cohort grew up. With more data, researchers could ask and answer different questions. They could now look at health over a longer span of time.
For example, Cohn and others who study Jennifer’s generation have learned that women who were exposed to a certain insect killer in the womb and during puberty are more likely to develop breast cancer in their 40s and 50s. That pesticide is called DDT. The U.S. government would go on to ban DDT over concerns that it was harming wildlife and posed a risk to human health.
Other cohort studies
The Child Health and Development Studies may be one of the longest running cohorts in the world. Yet it is not the only study to look into the role of the environment on health in different generations of the same families. Researchers in England, for instance, have been observing 14,500 families in the city of Bristol since 1991. They call this cohort the Children of the 90s study.
“We wanted to use the data we collected to generate hypotheses about how environment and genes impact a child’s brain development,” says Jean Golding. She’s a local epidemiologist who helped the study get its start. She works at the University of Bristol.
Findings from this cohort study have helped scientists form another hypothesis: that exposure of a fetus to toxic chemicals in the womb might harm later generations. And, Golding’s team showed, kids whose maternal grandmothers smoked while pregnant were slightly more likely to have autism than were kids whose maternal grandmothers didn’t smoke. However, this held only for kids whose moms also smoked while pregnant with them.
The Framingham Heart Study is another famous long-running cohort. It was designed to help scientists better understand what genetic and environmental factors can prove good — or bad — for heart health. It started in Framingham, Mass., in 1948, with 5,000 adults.
Researchers from around the world have published more than 3,500 science studies on the original Framingham adults, their children and their grandchildren. This study provided some of the first clues that cigarette smoking could contribute to heart disease. The study is now tracking a fourth generation.
Scientists need observations and experiments
Big studies such as the Framingham Heart Study and Child Health and Development Studies are rare. But they are very important. The CHDS program, for instance, allows researchers to study how lifestyle and environmental changes over time can play a role in disease, says Alessio Fasano. He’s a pediatric gastroenterologist. Such doctors study and treat diseases of the digestive tract in children. He works at Massachusetts General Hospital in Boston.

There, Fasano studies celiac (SEEL-ee-ak) disease. People with this disease are hurt by eating a substance called gluten (GLOO-ten). It’s found in breads and other foods made with certain grains. Few people knew about celiac disease in the 1950s and 1960s. It was rare. Now it’s on the rise. The number of new U.S. cases has doubled every 15 years since the 1970s. Doctors aren’t sure why. They think changes in the environment and in people’s lifestyle may have played a role. But they’re not sure what those changes might be.
Fasano’s team has started to look at data from the Child Health and Development Studies. His team is among those looking for changes to environmental exposures and lifestyles over the three generations. They hope that identifying such changes will help them better predict who is likely to develop celiac disease and why.
A new generation of people is born about every 20 years, on average. “Three generations ago we lived a completely different lifestyle,” says Fasano. “The environment was different. Now we can study how these changes impact health.”

As useful as cohort studies are, they have their limits. Scientists cannot use observational research to determine whether one particular thing causes something else. A cohort study might show that someone exposed in the womb to a certain pesticide gets breast cancer decades later. That’s a correlation. But correlations by themselves won’t prove the pesticides caused that cancer. There might be other explanations. To show causation, scientists need to do experiments that test their hypotheses.
Yet some experiments are hard to do in people. Some might even be unfair. If you have a strong suspicion that one chemical caused health problems, it would be unfair to make some people touch it or inhale it just to test your educated hunch. So scientists instead run such tests on cells, tissues or animals in a laboratory. These types of experiments can help researchers answer questions about how or why something happens.
Observation and experiment go hand in hand. “They work together to help researchers make and test hypotheses,” says Cohn.
Looking ahead
Isabel Katz now is a junior in college. There she is majoring in biology. A few years ago she was asked if, as an adult, she wanted to take part in the Child Health and Development Studies. She said yes, just like her grandma and mom had. “I knew that as a participant, I couldn’t be replaced,” says Katz.
Researchers now are beginning to collect data from Katz and other grandchildren of the original cohort members.
Consider the DDT exposures their grandmothers may have had. True, DDT is no longer used in the United States. But thousands of chemicals sold and used today that have been linked to an elevated risk of breast cancer and other diseases. Some of them have a chemical structure that is very similar to DDT. This suggests they might act similarly in the body, notes Cohn. “The hope now,” she says, is that with the coming cohort data, “we don’t have to wait another 60 years to study the long-term health effects [of such chemicals].”
The reporting for this story was supported by a Lizzie Grossman Freelance Grant for Environmental Health Reporting awarded through the Society for Environmental Journalism’s Fund for Environmental Journalism.







