Explainer: What is mpox (formerly monkeypox)?
Once rare, this viral disease exploded onto the global scene for the first time in 2022
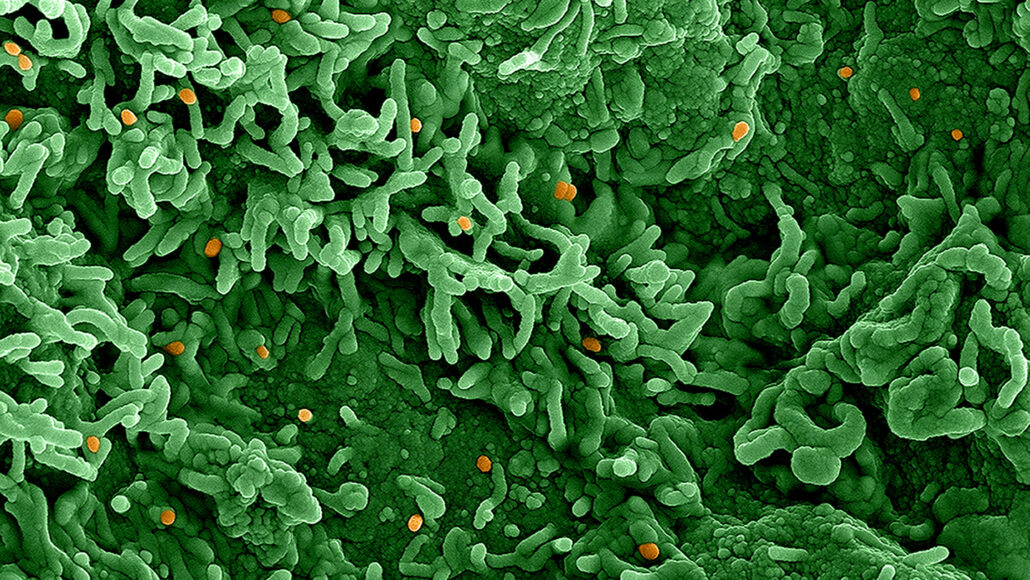
Monkeypox (orange) is infecting monkey cells (green) in this colorized electron micrograph. This virus belongs to the same family of germs as the smallpox virus and can be transmitted from person to person through contact with infectious particles.
NIAID/Flickr (CC BY 2.0)
By Tina Hesman Saey and Janet Raloff
Originally known as monkeypox, mpox is a viral disease best known for the sometimes itchy or painful rash it causes. People are worried about it because the disease can be deadly. It is especially dangerous for babies, elderly people, people with some skin diseases and people with weak immune systems.
Even for healthy people, however, mpox can be very painful and leave disfiguring scars.
Forest animals in Central and West Africa have been reservoirs for the virus. No one knew of the disease until 1958. That’s when the virus sickened two communities of monkeys that were being housed for research. The first human case would not show up until 1970. Since then, several large human outbreaks have arisen. Most occurred among communities in Africa.
All that changed in May 2022.
Suddenly, large numbers of people outside of Africa began showing symptoms of mpox. The start of the global outbreak was first noticed in the United Kingdom on May 6. Doctors reported the first U.S. case on May 17. By the end of May, the United Nations’ World Health Organization, or WHO, reported 257 confirmed cases and some 120 more suspected cases. These showed up among people in 23 countries. All lived outside of where the disease had commonly popped up before.
More cases continued to spread outside of Africa. On July 23, WHO labeled the fast-growing outbreak a “public health emergency of international concern.” By September 1, WHO had logged more than 50,000 cases around the world. At least 16 people have died, including one person in Texas. All but 443 cases were in places where monkeypox historically had not been seen.
What is monkeypox?
As with smallpox and cowpox, the virus behind mpox belongs to a genus known as Orthopoxvirus. Mpox spreads mostly through direct skin contact with either the skin of an infected person or with their spit or some other bodily secretion. Scientists are investigating if people without a rash can spread the disease. In fact, by late August 2022, there were signs that people can host the virus but show no symptoms.
The first signs of mpox tend to be flu-like. People may have fevers, chills, headaches, body and back aches, joint pain, fatigue, coughs and swollen lymph nodes. Those first symptoms usually show up within eight days of exposure to the virus. In some cases, symptoms may take more than two weeks to develop.
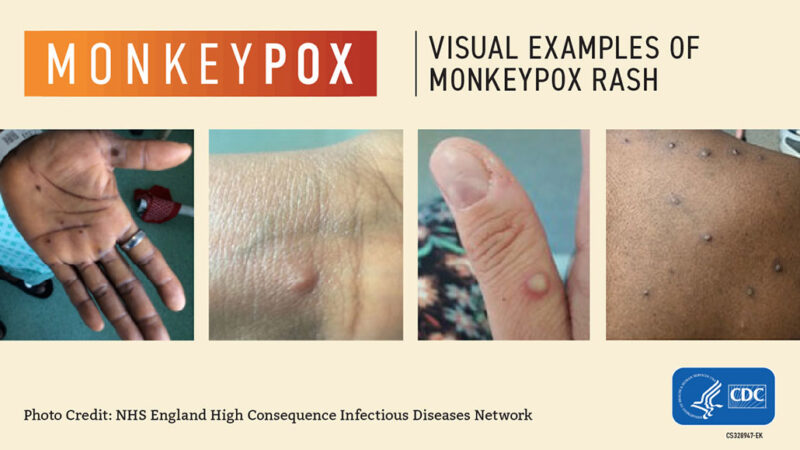
Any rash tends to emerge one to four days after those other symptoms. Flat spots on the skin eventually turn into pimples. These soon balloon into typical, pox-like blisters. Eventually, they’ll scab over, often leaving scars. Although people can die from mpox, the vast majority do recover.
A broad range of mammals can carry the virus, according to the U.S. Centers for Disease Control and Prevention. In Africa, the virus has been seen in rope and sun squirrels, giant-pouched rats and African dormice. Not all will show symptoms. A 2003 outbreak occurred in caged U.S. prairie dogs after they had been exposed to animals imported from West Africa. (This led to 47 cases of human disease spanning six U.S. states.) Larger primates, such as monkeys, can pick up the disease — and become visibly ill.
Adesola Yinka-Ogunleye is an epidemiologist. That’s a type of disease detective. She works at the Institute for Global Health. It’s in England at University College London. She’s also an mpox expert with the Nigeria Centre for Disease Control. Through 2016, mpox was a relatively rare disease, she notes. Fewer than 10 human cases had popped up in Western Africa. But then a 2017 outbreak in Nigeria caused 42 confirmed cases and 146 more suspected ones. The next year, Yinka-Ogunleye was part of a team that described that outbreak in Emerging Infectious Diseases.
She notes that there are two different variants — or clades — of mpox. The first, clade I, sickens hundreds of people each year in Congo and the Central African Republic. It also kills about 10 in every 100 people it infects. So far, this type of monkeypox hasn’t spread outside the region where it is normally found, Yinka-Ogunleye says.
A milder type known as clade IIb is behind the current global outbreak. It, too, can be life-threatening. Before the global outbreak, clade II killed between 1 and 4 in every 100 infected people. But the death toll in the 2022 outbreak has been lower than expected.
Treatments exist — and more may be coming
Before the global 2022 outbreak, Yinka-Ogunleye says, doctors controlled monkeypox in Nigeria by isolating infected people. Then they traced their close contacts to find other people who might be at risk. Vaccines and antiviral medications exist. However, she says, they have not been available in Nigeria to limit the disease’s impact or spread there. In fact, treatment often is not needed, she says. The body usually clears the virus on its own.
Outside of Africa, including in the United States, smallpox vaccines are being used against mpox. The shots can be given to people exposed to someone with mpox. The vaccine may keep the exposed person from getting the disease.
An antiviral drug that was developed to treat smallpox is also available in some places. Scientists and doctors aren’t sure how well it works against mpox. Human trials to test that were launched in late August 2022.
NOTE: This story has been updated to reflect a renaming of the disease by the World Health Organization in late November 2022. At that time, the agency announced: “Following a series of consultations with global experts, WHO will begin using a new preferred term ‘mpox’ as a synonym for monkeypox. Both names will be used simultaneously for one year while ‘monkeypox’ is phased out.”







