Explainer: Why it’s easier to get sick in the winter
Low humidity and cold weather can make catching a cold, the flu or COVID-19 more likely

In winter, it’s easier to catch colds, the flu and COVID-19. Cold, dry weather is partly to blame.
invincible_bulldog/iStock/Getty Images Plus
In the winter, my grandmother would urge me to come inside. “You’ll catch your death of cold out there,” she’d say.
Sure, freezing to death is possible in frigid temperatures. But my grandmother was worried about me catching an illness. Doctors stress that being cold won’t give you a cold. Still, winter is for sure cold-and-flu season. It’s also a time when COVID-19 spreads more.
But if the chill doesn’t matter, why do people get sick more in winter?
“I’ve spent the past 13 years looking into this question,” says Linsey Marr. As a civil and environmental engineer, Marr studies viruses in the air. She works at Virginia Tech in Blacksburg. “The deeper we go, the more I realize we don’t know [and] the more there is to figure out.”
Marr and I are not alone.
The spike in illness seen in winter “has puzzled people for a very long time. Thousands of years,” says Jeffrey Shaman. He is an infectious disease researcher based in New York City. He works at the Columbia University Mailman School of Public Health.
Winter’s shorter days may make people more prone to infection, he says. Less sunlight means people’s bodies make less vitamin D. That vitamin helps the immune system fight off disease. But that’s just one piece of the puzzle.
Scientists are also studying other things that make winter a sickening season.
Inside is where illness spreads more
By making me come inside, grandma may have actually increased the risk that I’d get sick.
Some viruses spread more when people spend more time indoors. Examples include colds, influenza and respiratory syncytial virus, or RSV. In places that have four distinct seasons, these viruses cause more illness in winter. They also spread more during rainy seasons in tropical zones. COVID-19 spreads more easily indoors than outside, too.
Why? These infections are caused by viruses that travel in small droplets. Such droplets are a type of aerosol. They can be released into the air when sick people exhale.
“Outdoors, you’re in the ultimate well-ventilated space,” says David Fisman. He is an epidemiologist in Canada. He works at the University of Toronto Dalla Lana School of Public Health. Viruses exhaled outdoors quickly mix with clean air, he explains. This dilution makes it harder for the viruses to reach people.
But inside, aerosols — including any viruses — can build up. “The air you breathe in is often air that other people have breathed out,” Fisman says. Being close to contagious people could increase your chance of getting sick.
But being inside can’t be the whole reason people tend to get sick in winter, says Benjamin Bleier. He is a doctor who specializes in sinus and nasal disorders. He works at Harvard Medical School in Cambridge, Mass. “In modern society, we’re indoors all year round,” he says. So to drive the seasonal pattern, he says, something else must be going on. Bleier thinks people must become more prone to infection in winter. And the amount of virus circulating must go up, he says.
Some viruses spread better in drier air
Some viruses thrive in winter. The reason may not be cold temperatures but low humidity (low levels of moisture in air).
Take flu viruses and SARS-CoV-2. That’s the coronavirus that causes COVID-19. Those viruses survive best when the relative humidity falls below about 40 percent. Marr and other researchers made that discovery.
Viruses are sensitive to humidity because they aren’t usually floating around naked, Marr explains. They are encased in droplets of fluid (think spit or snot) — which can dry up in low humidity. Those droplets also have bits of mucus, proteins, salt and other substances in them. Those other components may determine if the virus survives drying.
When the humidity is higher, droplets dry slowly. Such slow drying concentrates salt and other things in the droplets that can harm a virus. That kills viruses such as influenza A and SARS-CoV-2. Marr and her colleagues reported that finding last July in a paper posted on bioRxiv.org. (Studies posted there have not yet been vetted by other scientists.)
Meanwhile, in low humidity, droplets dry fast. That flash-drying in parched air preserves viruses. “If the air is very dry, the water quickly evaporates. Everything is dried down, and it’s almost like things are frozen in place,” Marr says.
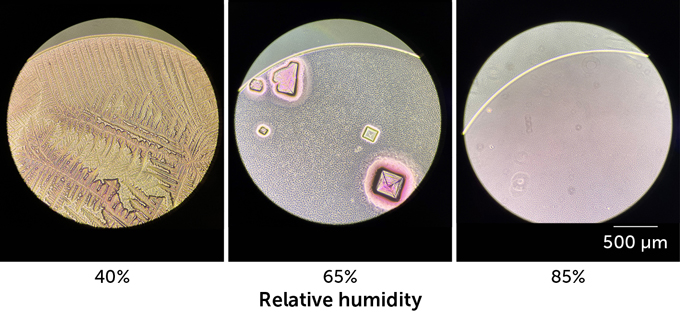
How humidity affects droplets in the air
Viruses often travel through the air inside airborne droplets, or aerosols. When the air is dry, aerosols dry quickly (left). This drying encloses viruses in a layer of crystals that look like feathers (as this microscope image shows). That flash-drying protects viruses, although scientists don’t know exactly how. At medium levels of humidity, crystals form inside liquid droplets (middle). Those crystals may inactivate viruses, not protect them. At high humidity levels (right), aerosols remain liquid. This also allows viruses to survive better than at mid-level humidity.
Drier, smaller aerosols also are more buoyant than large droplets. So, those aerosols can hang in the air longer. That ups the chance someone will be able to breathe them in, Fisman says.
What’s more, dry air can tear down some of our defenses against viruses. Dry air can trigger the death of some cells lining the airways. That could leave cracks where viruses can invade. Scientists know this from studies in lab animals.
Mucus in the airways can trap viruses and help protect against infection. That mucus carries germs out of the body through a runny nose or hacked-up phlegm. But breathing cold, dry air can slow the system that moves mucus out of the body. That slowdown may give viruses time to break out of the mucus trap and invade cells, Fisman says.
The bubble trick — compromised?
Temperature changes can also impact the immune system — an important defense against disease.
Normally, the immune system employs a trick to help ward off viruses. Bleier is part of a team that recently discovered this trick. Cells in the nose are studded with surface proteins that can detect viruses. Other cells in the body also have virus sensors. When one of these sensor proteins sees a virus coming, it signals the cell to release tiny bubbles. Those bubbles — called extracellular vesicles — work as decoys. Viruses may go after them instead of infecting real cells.
The virus that docks with one of the bubbles is in for a surprise. Inside the vesicles are virus-killing bits of genetic material. They’re called microRNAs. One type of microRNA in the bubbles is known as miR-17. It can kill multiple types of cold-causing viruses. Bleier’s team shared those findings December 6, 2022, in the Journal of Allergy and Clinical Immunology.
Cold temps may impede the body’s ability to make such virus-killing decoy bubbles. Bleier’s team grew human nasal cells in lab dishes at 37° Celsius (98.6° Fahrenheit). That is our typical body temperature. The researchers measured how many bubbles the cells released. Then, the scientists lowered the thermostat to 32° C (89.6° F). Cells released about 42 percent fewer bubbles at the cooler temperature. What’s more, those vesicles carried fewer virus-killing weapons. Vesicles can pack in about 24 percent more microRNA at body temperature than when it is cooler.
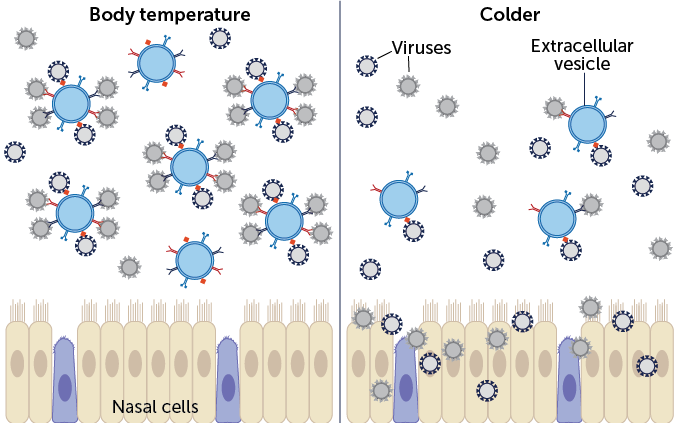
How cold weather weakens the immune system
The body’s immune system uses a clever trick to keep viruses from infecting cells in the nose. When the body detects viruses (black and gray spheres), cells in the nose release bubbles (blue circles). These bubbles are called extracellular vesicles. The bubbles sport proteins (red, blue and black shapes on blue circles) like ones found on nasal cells. This makes them effective decoys: Viruses may go after the bubbles instead of infecting real cells. But when it gets cold (right), cells release fewer bubbles. This makes it easier for viruses to find and infect real nasal cells.
Three tips to fend off viruses
What can people do to protect themselves from viruses in the winter? Some experts suggest using a humidifier to raise moisture levels in the air. If they raise it high enough, that might slow the drying of airborne droplets. Such a slow drying might help kill any viruses in the droplets.
“Any increase in humidity should be beneficial,” says Shaman. “You get a lot of bang for your buck if you go from very dry [air] to dry.”
But Donald Milton doesn’t think it’s a good idea to pump a lot of moisture into a house when it is cold outside. “That humidity is going to find … cold spaces in your house and condense there.” Condensation creates a breeding ground for mold and rot, says Milton. He studies viruses in the air. He works at the University of Maryland School of Public Health. That’s in College Park.
Instead of boosting humidity, Milton advises turning on kitchen and bathroom exhaust fans. That boosts ventilation. And use HEPA filters or Corsi-Rosenthal boxes. They filter unwanted viruses out of the air.
Bleier suggests wearing a mask. Masks don’t just filter out viruses. “Our work suggests these masks have a second mechanism of action,” he says. “They keep a cushion of warm [moist] air in front of our noses, which could help bolster the immune system.”







