Patches and robotic pills may one day replace injections
These alternate methods to deliver medicine could be more patient-friendly
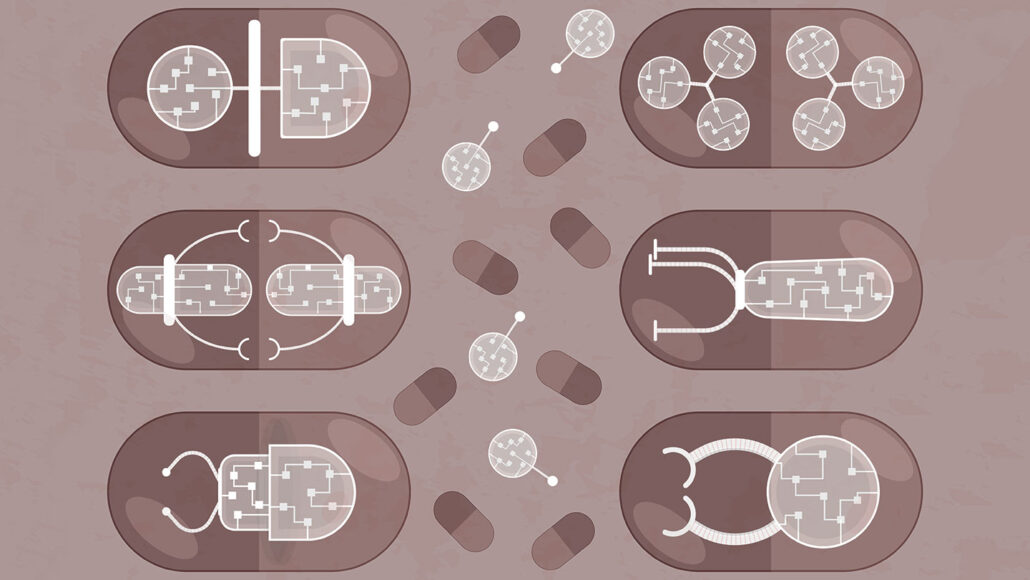
Robotic pills may one day provide alternatives to conventional injections. This conceptual art imagines different designs for how futuristic mechanical pills may be structured.
Valentina Kruchinina/iStock/Getty Images Plus
Do you hate getting shots? If so, you’re not alone — and you may be in luck. Researchers are devising new, pain-free ways to deliver drugs. One is a robotic pill. Another is a medicine patch worn on the skin. Both are still in the early stages of development. But someday, these innovations could make delivering medicines more patient-friendly.
The new robotic pill comes out of a lab at the Massachusetts Institute of Technology in Cambridge. It holds a teeny, spring-loaded microneedle only about 3 millimeters (a tenth of an inch) long. Once swallowed, the pill injects medicine directly through the stomach wall.
Unlike a normal shot, this needle prick shouldn’t hurt, says Giovanni Traverso. He’s a physician and biomedical engineer who specializes in the gut. He also helped develop the robo-pill at MIT. Stomachs can detectsome sensations, such as the deep ache of a stomach ulcer. Or the discomfort of feeling bloated. But those sensations are “more related to stretch receptors,” Traverso explains. The stomach lacks receptors to detect sharp pains, such as an injection.

Designing a pill that could reliably prick the stomach wall was a bit tricky. Once swallowed, the small but heavy device settles to the bottom of the stomach. In order to prick the stomach wall beneath it, the pill must land injector-side-down. To make that happen, the MIT team borrowed an idea from the leopard tortoise.
Contrary to popular belief, most tortoises can get back on their feet if flipped upside-down. Leopard tortoises are aided by steeply domed shells. If one of them is flipped on its back, the shape of that shell helps it roll right-side up. That same shape ensures the new pill always lands upright, too.
Robert Langer is a chemical engineer on the MIT team. “Watch,” he says, as he drops a chickpea-sized robotic pill onto a table. It bounces, then rolls upright. “No matter how I drop it,” he notes — and he drops it again — “it always lands the same way.”
But what makes the pill’s tiny needle pop out to do its job? “Sugar glass,” Langer explains. Hard and brittle, this material holds back a spring that is attached to the needle. In the stomach, that sugar starts to dissolve. “All of a sudden, the thing breaks,” Langer says. This releases the spring, which jabs the needle into the stomach wall to inject medicine. It’s possible to control when that happens by adjusting the sugar’s thickness.
The MIT team unveiled its design in 2019 in Science.

Potential perks and pricing
In new experiments, these robotic pills have delivered an mRNA-based medicine to mini-pigs. The researchers described their success in the March 2 issue of Matter. It was an important test for showing that this new class of medicines could be delivered in this way. (Pfizer’s COVID-19 vaccine also relies on mRNA.)
The new robo-pills also have successfully delivered insulin in mini-pigs. Many people with diabetes must inject themselves several times a day with this hormone. Normally, insulin cannot be swallowed as a pill because it would break down in the stomach. The robo-pill gets around that problem by feeding insulin straight into the stomach wall.
This is a completely new way to deliver the drug, notes Bruno Sarmento. He works at the University of Porto in Portugal. Although he didn’t work on the pill system, as a nanomedicine researcher he’s interested in such projects. “We know now that it’s possible” for a robotic system to reach the stomach and deliver injections, he says. But he worries that the new pill may be too expensive for widespread use.
Langer isn’t so sure. “I actually don’t know that it’ll be that expensive,” he says. Mechanized pills already exist. Langer points to a class known as osmotic pills. These pills have holes in them to pump drugs out. People might think they’d be a lot more expensive than regular pills, “but they really haven’t been,” he says. “When you start to make billions of these, the cost just goes way down.”
What’s more, normal pills often waste medicine. A swallowed drug must pass through the stomach lining. “That’s like going through a brick wall,” Traverso says. It’s very difficult without the help of a needle. And wasted drug is expensive — “sometimes more expensive than the device.”
One example is a drug used to treat diabetes. It’s called semaglutide. “It’s a giant seller for people with diabetes,” Langer says. And when you give this medicine as a pill, he says, “you lose 99 percent of the drug.” It passes through the body before it’s absorbed. But the new robo-pill would ensure the drug makes it right through the stomach wall and into the bloodstream. In the end, that could save money.
After successful tests in animals, the robo-pill is now ready for human trials. The Danish pharmaceutical company Novo Nordisk, which works with the MIT team, started recruiting volunteers in April.
Patching the skin
Researchers in France are developing a technology that skips needles altogether. The team’s new patch, when applied in the mouth, delivers a drug through the inside of the cheek.
“Needle-less injections … it’s kind of the holy grail,” says Karolina Dziemidowicz. She did not help create the new patch. But her work in England at University College London does focus on such new biomaterials.

Sticky, medicine-loaded patches have been around for decades, Dziemidowicz notes. This new one is different. Rather than sticking it on your arm, it goes onto the slippery, mucus-coated membrane inside your mouth. Or even your eyeball! Both are areas that let medicines quickly enter your bloodstream. Gentle heat from a laser device activates the patch to release the medicine.
Sabine Szunerits is an analytical chemist and co-developer of these tiny patches. She works at the University of Lille in France. Her team tested these patches as a way to dispense insulin. Like the MIT team, they tried their system out in mini-pigs — and later, in cows. The animals absorbed the drug well, and it reduced their blood sugar as intended.
In another experiment, the researchers even applied drug-free versions of the patches inside the mouths of six volunteers. What did people think of them? It’s weird to think about, two male volunteers said. But nobody found the patches uncomfortable. Nor did the patches affect the volunteers’ ability to talk or eat.
Szunerits and her team described their findings in ACS Applied Bio Materials on February 21.
New tech, new things to consider
In its lab, the French team used a laser to make the patch release its drug. For home use, Szunerits imagines creating something like a lollipop. At its end, she says, “you’d have a laser.” Then, when you’re ready to activate a patch, you’d put the laser-pop in your mouth. You could trigger just one — or as many patches as you need to take the prescribed dose.
“This is a very elegant study,” Sarmento says. But he sees a limitation. The patches can’t provide very much insulin. Each one can pack about 2.9 units of the medication. But even a 40-kilogram (90-pound) child might need about 20 units of insulin per day. Sarmento suspects the new patch might be better suited for other drugs — ones given at lower doses.
The patches are small, but some people might be willing wear a bunch if it means avoiding an injection. People, especially kids, dislike shots. Because of that, Traverso says, many people reliably take their insulin only about half the time. That’s why many “physicians delay starting people on insulin by almost eight years,” Traverso says.
He now hopes innovations like the insulin patch and robotic pill might one day get more people to willingly take the meds they need.
This is one in a series presenting news on technology and innovation, made possible with generous support from the Lemelson Foundation.







