Medicine Nobel honors discovery of how cells deal with oxygen
The finding may one day lead to new medicines, such as for treating cancer
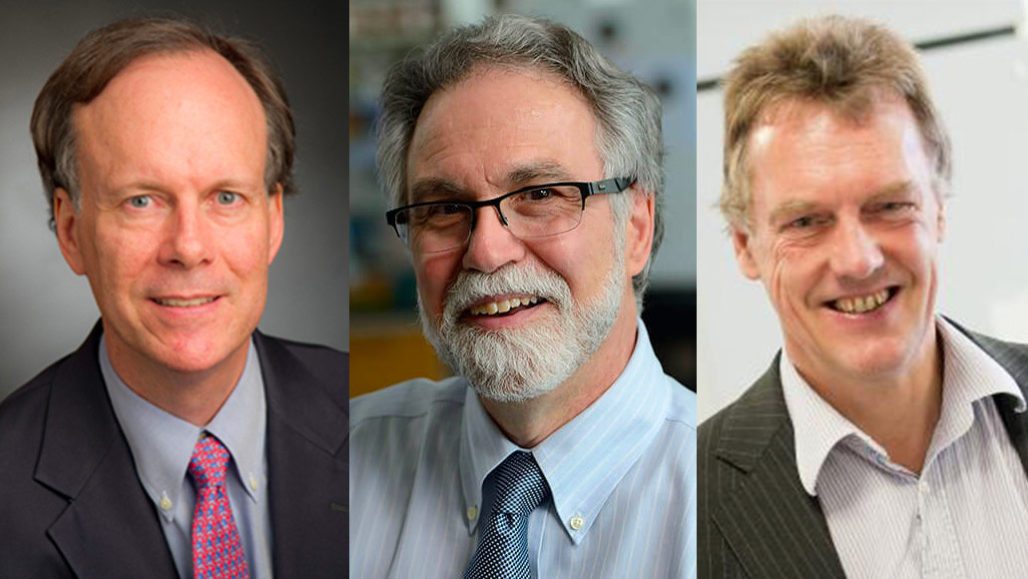
The trio of winners for this year’s Nobel Prize in physiology or medicine are (left to right) William Kaelin, Gregg Semenza and Peter Ratcliffe. They discovered the molecular machinery that allows cells to sense and respond to changes in oxygen levels.
FROM LEFT: DANA-FARBER; JOHNS HOPKINS; UNIV. OF OXFORD
By Tina Hesman Saey and Aimee Cunningham
Like candles or furnaces, cells need oxygen to function correctly. If oxygen isn’t regulated properly, cells could die. Three physician-scientists learned today that they had won the 2019 Nobel Prize in physiology or medicine for their work on how cells sense and respond to this oxygen.
Gregg Semenza works at the Johns Hopkins University School of Medicine in Baltimore, Md. William Kaelin is a cancer biologist at the Dana-Farber Cancer Institute in Boston, Mass. Peter Ratcliffe works in England at the Francis Crick Institute in London. Each made pivotal discoveries relating to the HIF system. This system is made up of proteins that tell cells how much oxygen is around. It also helps keep cells from suffocating when there is too little oxygen. That HIF system plays a role in anemia, cancer, heart attack, stroke and other disorders.
The trio’s discoveries were made in the 1990s. But it often takes decades before the Nobel Assembly chooses whom to honor. It may wait for “the year when the full impact of the discovery has become evident,” according to the late Ralf Pettersson, who once chaired the Nobel selection committee. It’s part of the Karolinska Institute in Stockholm, Sweden.
Nobel committee member Randall Johnson took part in announcing who the Nobel Assembly chose to honor this year. He says the three researchers’ work has the potential to impact nearly every aspect of physiology (how the body works). It spans from metabolism and exercise, to immunity, the development of embryos and how the body deals with low oxygen concentrations at high altitudes.
“It’s very clear that we now understand this,” said Johnson. It works like a fundamental biological switch. And at last, he noted, “It seems like a complete and clear story.”
“Life as we know it wouldn’t exist without oxygen,” points out Dennis Brown. He’s a cell physiologist in Boston at Massachusetts General Hospital and Harvard Medical School. For many years, scientists understood that cells could adjust to differing levels of oxygen. However, Brown notes, no one knew how cells did it — until Semenza, Kaelin and Ratcliffe made their discoveries.
The three researchers will split the prize of 9 million Swedish kronor, or more than $900,000.

How their findings came together
Semenza and Ratcliffe each discovered that all cells can sense when oxygen levels drop. “Your body does all sorts of things to keep the level of oxygen appropriately high in your blood and in your tissues,” says Andrew Murray. He’s a cell biologist at Harvard University. At high altitudes, where the air is thinner, the body can’t get enough oxygen. Blood levels of this gas fall. This creates a condition known as hypoxia. And when this occurs, the kidneys respond by making a protein that works as a hormone. It’s known as erythropoietin (Ee-REETH-roh-POY-eh-tin). Often called EPO, it signals the bone marrow to make red blood cells. These blood cells contain hemoglobin, which ferries oxygen throughout the body. So making more red blood cells boosts the amount of oxygen the body can deliver to cells and tissues.
Semenza went on to identify HIF — short for hypoxia-inducible factor. This is a group of proteins that function as a switch. It turns on the activity of the genes needed to make EPO and other proteins. And in doing that, HIF helps cells attempt to cope with low-oxygen conditions.
Ratcliffe is a kidney physiologist, an expert in the function of the kidneys. He discovered that cells constantly make HIF proteins. However, notes Murray, if there is enough oxygen, cells promptly chew up those proteins. HIF and other proteins slated for destruction get tagged with an “eat me” sign, he says. That sign consists of a small protein called ubiquitin (Yu-BIH-quih-tin).
At about the same time as Ratcliffe made his finding, Kaelin was studying an inherited cancer. People with this von Hippel-Lindau (VHL) disease often have tumors in their pancreas, kidneys and adrenal glands. They also can have tumors in the central nervous system (brain and other nerve tissues).
Nervous-system tumors may resemble tangles of blood vessels. Sometimes these tumors produce the same distress signals as cells that are low on oxygen. Kaelin discovered that proteins known as the VHL complex (because they go awry in these cancers), help hang that “eat me” tag on HIF. And that’s what triggers HIF’s destruction.
Kaelin probed how VHL knows when to tag HIF and when to leave it alone. When oxygen levels are normal, HIF sports hydroxyl groups (a hydroxyl group is a molecule, OH, made with an atom of oxygen and an atom of hydrogen). The hydroxyl groups are the signal for VHL to launch HIF’s breakup. When oxygen is low, hydroxyl groups don’t get added and VHL ignores it. This allows HIF to turn on creation of EPO and other proteins needed to survive low levels of oxygen.
Importance of these findings for medicine
Mutations are spontaneous changes to genes. Some mutations that inactivate VHL increase HIF levels. When this happens, cancer cells can boost their oxygen-scavenging activities. It helps tumors fuel the growth of new blood vessels. That process is known as angiogenesis (AN-gee-oh-JEN-eh-sis). It helps supply tumors with the energy they need to keep growing.
Indeed, the robust growth of cancer cells would quickly exhaust a tumor’s oxygen supply without these new blood vessels. Explains Murray, oxygen can diffuse only about half a millimeter away from a tiny blood vessels before the cells around it use up that oxygen. So to grow more than about 1 millimeter across, tumors must continue to make new blood vessels.
Some researchers are working on treatments to suffocate cancer cells by switching off their HIF system. Turning on low-oxygen responses also might help limit damage from heart attacks or kidney disease, Brown says.
A new drug known as roxadustat can control the HIF system. It has been approved in China to treat anemia in patients with chronic kidney disease. People with this condition get anemia when their kidneys fail and no longer make enough EPO. Roxadustat blocks the enzymes that normally break down HIF. That keeps this switch on to increase EPO levels and the production of red blood cells.







