RNA work that led to COVID-19 vaccines wins 2023 Nobel in medicine
Katalin Karikó and Drew Weissman overcame hurdles that enabled creation of mRNA vaccines
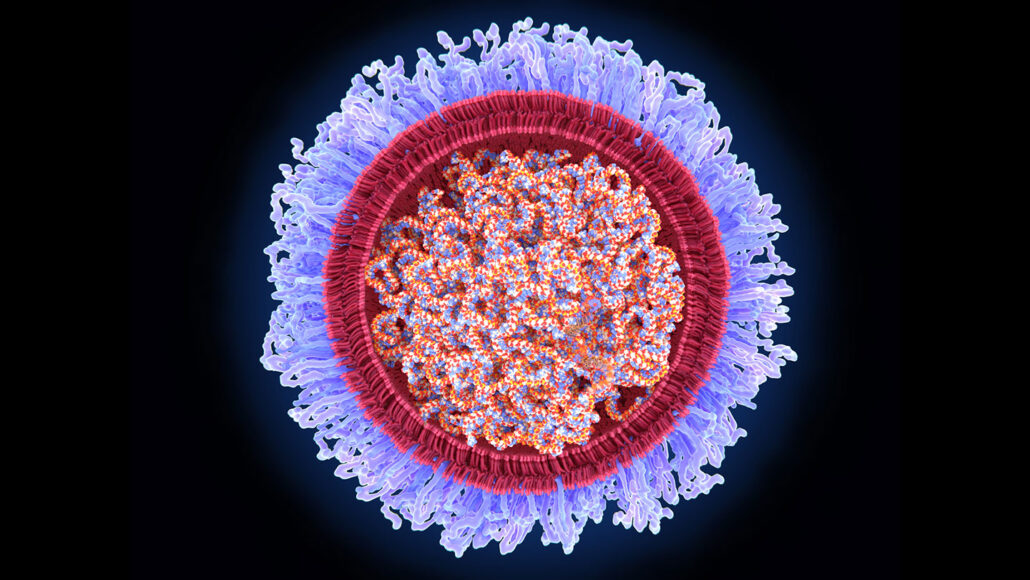
Together, Katalin Karikó and Drew Weissman discovered how to safely deliver mRNA into cells of the body. They started by tweaking mRNA so that it wouldn’t spark a bad reaction from the body when it was injected. Then they jacketed the modified molecule inside lipid bubbles (illustrated).
JUAN GAERTNER/SCIENCE PHOTO LIBRARY/GETTY IMAGES
Listen to this story:
Have feedback on the audio version of this story? Let us know!
In December 2020, the first vaccines based on a type of genetic material known as mRNA rolled out to fight COVID-19. That was less than 12 months after the lethal disease came to the world’s notice. Within a year, those new shots appeared to have saved nearly 20 million lives. Now, two biochemists who laid the groundwork for mRNA vaccines have been awarded the 2023 Nobel Prize in medicine or physiology.
They’re Katalin Karikó and Drew Weissman. Both have spent many years working in Philadelphia at the University of Pennsylvania, or Penn. Now Karikó is at the University of Szeged in Hungary (her native country) as well as at Penn. On Oct. 2, the pair learned they are sharing a Nobel for modifying mRNA in a way that makes it useful in medicine.
Ultimately, their work could lead to other vaccines and to treatments for other infectious diseases and cancer.
It’s no exaggeration to say the COVID-19 pandemic “was a traumatic event,” said Qiang Pan-Hammarström. She’s a member of the Nobel Assembly at the Karolinska Institute. It’s in Stockholm, Sweden. Her group awards the prize for medicine or physiology. The basic discovery by these two scientists “has made a huge impact on our society,” she says. Pan-Hammarström shared her comments after an Oct. 2 news briefing that named the winners.
As of March 2023, more than 13 billion jabs had delivered COVID-19 vaccines into the arms of people around the globe. In the United States, mRNA shots accounted for the vast majority of COVID vaccinations. There, the vaccines are believed to have prevented some 1.1 million COVID-related deaths and 10.3 million hospitalizations.
A different type of vaccine
RNA is DNA’s lesser-known chemical cousin.
DNA contains the genetic instructions for what the body’s cells should do. To carry out those tasks, cells start by making RNA copies of the DNA instructions. Some of the copies — known as messenger RNA, or mRNA — will be used to build proteins.
Proteins do much of the important work that keeps cells (and the organisms they’re a part of) alive and well. Messenger RNA “literally tells your cells what proteins to make,” says Kizzmekia Corbett-Helaire. She works at the Harvard T. H. Chan School of Public Health. It’s in Boston, Mass. There, she studies how viruses and the immune system interact.
Most vaccines inject something into the body to prod the immune system into making protective antibodies and other defenses against future infections. Those prodding agents could be viruses or bacteria that have been weakened or killed. They also could be some protein made by those germs.
The mRNA vaccines are different. They don’t contain a virus or part of a virus. Instead, they inject mRNA that carries the instructions to make a protein from the target virus.
When someone gets this shot, the mRNA gets into their cells. This triggers those cells to make the viral protein — but just for a short time.
The vaccine “tells the body to do things that the body already does, except now we make an extra protein,” explains Corbett-Helaire. That lets scientists skip a step. Otherwise, they would have to make proteins in the lab. Then the proteins would be given in a vaccine. It’s easier, she says, to instead give a shot of mRNA and let the body make the needed protein.
As the person’s immune system encounters this protein, it builds defenses. If that person later gets infected with the coronavirus that causes COVID-19, those defensive agents will now assault the virus.
Pfizer/BioNTech and Moderna made the first approved mRNA vaccines against COVID-19. One day, mRNA vaccines also may be unleashed against other diseases, including some rare genetic diseases. Human trials are even underway for some of these.

A long time coming
Karikó and Weissman’s partnership began in 1997. They met over a copying machine at Penn. Karikó would go on to tell Weissman about her work with RNA. He shared with her his interest in vaccines.
Although they worked in separate buildings, they eventually collaborated to solve a fundamental problem. Pumping normal mRNA into the body gets the immune system riled up — and in a bad way. It triggers a flood of immune chemicals that can turn on damaging inflammation. What’s more, this mRNA produces very little immunizing protein after being injected into the body.
But the researchers found a way around these problems. They started by swapping out one building block of RNA — uridine — for a tweaked version of the molecule. This dampened the bad immune reaction, the team reported back in 2005.
“The messenger RNA has to hide and it has to go unnoticed by our bodies (which are very brilliant at destroying things that are foreign),” Corbett-Helaire says. Those new tweaks proved important to helping the mRNA “hide while also being very helpful to the body.”
When injected in the body, their tweaked mRNA now produced lots of protein. This caused the immune system to build defenses against a target virus. The researchers shared their findings in 2008 and 2010.
This tweaking of mRNA’s building blocks is what the 2023 Nobel Prize honors.
Giving RNA its due
For years, “we couldn’t get people to notice RNA as something interesting,” recalled Weissman. He spoke at an Oct. 2 news conference at Penn. In the early 1990s, vaccines using the new technology failed several human trials. Most researchers gave up on it.
But then Karikó “lit the match,” Weissman said. “We would talk about all the things that we thought RNA could do,” he recalled. Together, he said, they realized “how important it had the potential to be. That’s why we never gave up.”
Along the way, Karikó and Weissman started a company. Called RNARx, it aimed to develop mRNA-based treatments and vaccines.
Karikó later joined the German company BioNTech. But she and Weissman continued to work together. In 2015, they were part of a team that encased mRNA in bubbles of lipids, which are fatty compounds. This helped keep the body from breaking down the fragile RNA before it could get into cells.
The researchers then began developing their first mRNA vaccine — for Zika. Suddenly, the COVID-19 pandemic hit. At once they changed their focus. They now applied all they had learned to making a vaccine against COVID-19.

Struggles to gain acceptance
Thomas Perlmann is Secretary General of the Nobel Assembly at the Karolinska Institute. He asked the two winners if they were surprised to get a Nobel. Karikó, he said, was overwhelmed.
Just 10 years ago, she told him, she was let go from her job. She had to move to Germany without her family to find work. And the U.S. National Institutes of Health never supported her research.
“She struggled and didn’t get recognition for the importance of her vision,” Perlmann said on October 2. Still, she had a passion for using mRNA in medicine. “She resisted the temptation to sort of go away from that path and do something maybe easier.”
This award shows that “there are just a million other possibilities for messenger RNA … beyond the vaccines,” Corbett-Helaire says.
Nobels have been awarded since 1901. Karikó is the 61st woman to win one — and only the 13th to get one in physiology or medicine.
Karikó and Weissman will share a prize of 11 million Swedish kronor. That’s equal to roughly $1 million.







