New date for U.S. arrival of the AIDS virus
HIV started circulating at least a decade earlier than previously realized, new DNA data show
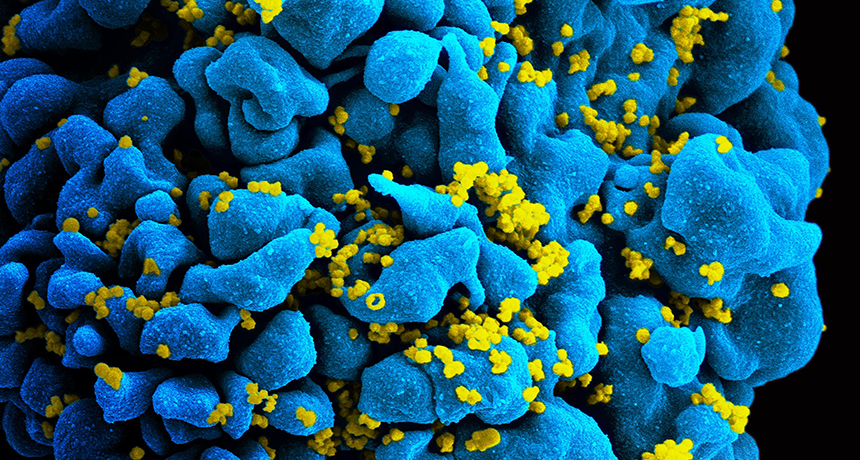
The HIV virus is shown here in yellow, infecting a T cell (blue). New data show that the virus first hit American shores in about 1971. It entered the Caribbean, then arrived in New York City and then spread elsewhere.
NIAID
Who first brought the human immunodeficiency virus — or HIV (also known as the AIDS virus) — to the United States? For years, people have pointed to a Canadian flight attendant as “Patient Zero.” That’s the term health-care officials give to the first case. But this man was not to blame, a new genetic study finds. The virus was actually circulating around New York City years before that flight attendant first came to the country.
For their new study, researchers used genetic tools that had been developed to decipher badly degraded DNA from ancient fossils. They used the technique on viruses that had been collected from people in the 1970s and stored away.
That analysis now shows that HIV was already infecting people in New York City between 1969 and 1973. That’s before the man alleged to be Patient Zero first arrived on the scene.
Michael Worobey works at the University of Arizona in Tucson. As an evolutionary biologist, he uses microbiology and genetics to study how microbes and other organisms have changed and adapted over time. He and his colleagues figured out the genetic instruction books of eight HIV viruses. They were isolated from blood samples collected in 1978 and 1979. Some came from New York City, the others from San Francisco, Calif.
The viral DNA was genetically diverse. That means that the type in one virus did not look identical to that in another’s. For that to be true, the viruses must have been circulating in these cities for years, changing a bit every time they made copies of themselves.
Worobey’s team now calculates that the virus likely first entered the United States in 1970 or 1971. HIV must have spread, therefore, for about a decade before AIDS was recognized in 1981. By 1983, scientists identified the virus causing this deadly infection. It would soon be known as HIV. By 2012, more than 1.2 million people in the United States had been infected. Worobey’s team reported its new discovery October 26 in Nature.
HIV comes to America
The new genetic analysis shows that HIV spread from Africa to the Caribbean in the 1960s. From there it moved into New York City (see map) around 1970 or 1971. Afterward, the virus spread to other parts of the United States.
Exactly how the virus was carried from the Caribbean to New York isn’t known. At the time, many blood products used in the United States came from Haiti. So infected blood products could have spread the virus to several people at once. Hemophiliacs are people whose blood doesn’t clot properly. They often need to get transfusions of blood products to help. Between the 1970s and mid-1980s, about half of all hemophiliacs were infected. Afterward, scientists developed ways to kill the virus in blood before it would be shared.
Other people who got blood during surgeries or for other reasons also got infected sometimes. Those people could then have spread the virus they didn’t know they had. Americans visiting Caribbean islands also could have unintentionally brought the virus home with them. Or people from the Caribbean who didn’t know they were infected may have brought the virus when they visited New York. All are possible routes of spread.
People can also catch the virus from sharing needles or being stuck with an infected needle. Mothers can pass the virus to their babies during birth or through breast milk. Sex with an infected person is another way the virus spreads.
Story continues below map.
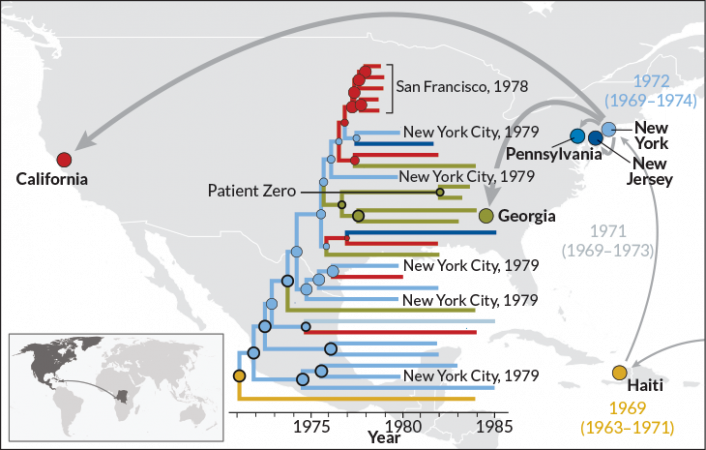
The New York HIV samples (see map, blue) were more diverse than those from California (pink). That told the scientists that the New York strain had more time to make copies of itself and pick up changes. More changes mean that a virus is older than one with fewer changes. So the researchers conclude that New York City was probably the hub of the early spread of HIV. Only later would the virus arrive in San Francisco.
Worobey and colleagues also examined the DNA in HIV from the man long thought to be Patient Zero. He was part a 1984 study of gay men with AIDS in Los Angeles. All had either a rare cancer, called Kaposi’s sarcoma, or a type of pneumonia frequently associated with AIDS. Researchers from the Centers for Disease Control and Prevention found that many of the men had had sexual contact with each other. This would help to show that HIV could be transmitted through sex.
Patient Zero’s origin
That 1984 study had referred to case number 57 as the center of a cluster of AIDS cases (see diagram). Three years later, in the book And the Band Played On, author Randy Shilts identified that man as Gaëtan Dugas.
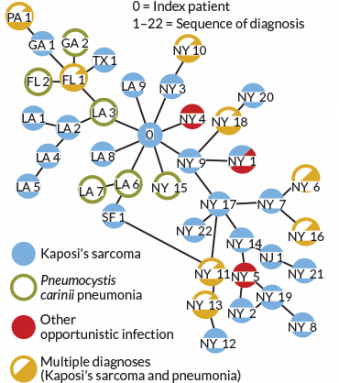
A mistake gave Shilts and others got the idea that Dugas started the AIDS epidemic in America. The 1984 paper didn’t identify people by their names. Instead, it gave them letters and numbers. For instance, LA9 meant that a man was the ninth case diagnosed in Los Angeles. And NY3 was the label given to the third case in New York. Dugas was called Patient “O” because he came from “Outside California.” But some people read the letter O as a zero. Shilts heard the term Patient Zero and thought it sounded catchy, so he used it in his book.
After that, the term Patient Zero came to mean the first person to catch an infectious disease and start an outbreak. So a typo caused people to accuse Dugas of bringing HIV to the United States.
Dugas became a flight attendant in 1974. Shortly afterward, he began traveling to the United States, notes Richard McKay. He’s a coauthor of the new study. He also is a medical historian at the University of Cambridge in England. Dugas estimated that he had sex with about 250 men each year between 1979 and 1981. Shilts and others argued that Dugas was intentionally spreading the virus to other men. In fact, Dugas couldn’t know. No one would know what AIDS was — or even that it was caused by a virus — for several more years.
Authors of the 1984 study repeatedly denied Dugas was the source of the U.S. AIDS epidemic. And the new analysis shows that his HIV strain came from a later branch of the HIV family tree (see map, green) than the New York and San Francisco strains. “This individual was simply one of thousands infected before HIV/AIDS was recognized,” McKay says.
The new study is a cautionary tale. It argues against trying to pin the spread of an infectious disease on any one person, says Robert Remien. He’s a behavioral scientist at Columbia University Medical Center in New York City. For many diseases, including HIV/AIDS, there may be no Patient Zero. Instead, lots of people spread the virus to others without knowing it, Remien says. “There’s no blame or cause to be laid on any of those people in those early years.”







