Scientists watch germs evolve into superbugs
Growth patterns on a giant plate of goo revealed how quickly they develop drug resistance
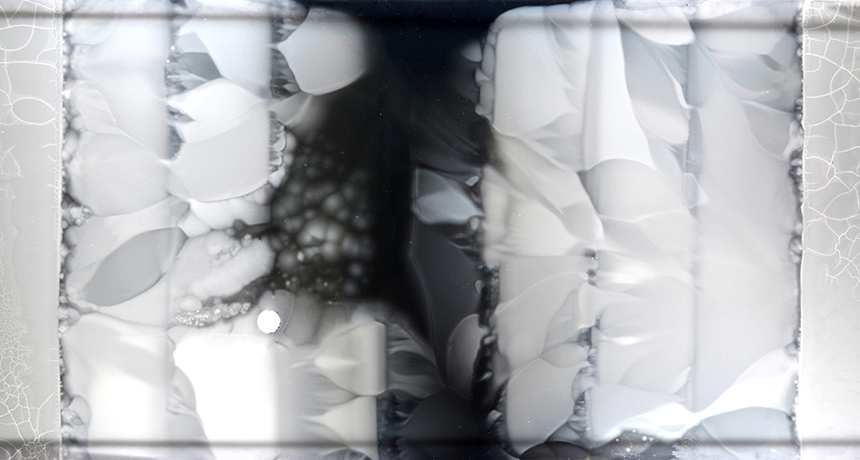
A giant plate of food more than a meter (yard) long helped scientists watch bacteria overcome the killing effects of antibiotic drugs. Bacteria placed on the outer edges had to adapt to higher and higher levels of the drugs as they spread toward the center.
Harvard Medical School
Germs are everywhere. Fortunately, most pose no risks to people. And those that do cause disease usually can be killed with antibiotic drugs. Sometimes, however, harmful bacteria evolve ways to “laugh at” antibiotics — survive as if the poisons were not even there. This so-called drug resistance make infections hard, if not impossible, to treat. How bacteria learn to resist killer drugs normally is invisible. But scientists have just unveiled a new tool that lets them watch it happen, right before their eyes.
“As someone who’s studied evolutionary biology for a long time, I think it has a real wow factor,” says Sam Brown. He is a microbiologist at the Georgia Institute of Technology in Atlanta. Brown applauds those who developed this new tool. Looking at it, he says, is like watching bacteria “climbing this impossible mountain of antibiotics.”
Antibiotic-resistant germs don’t look any different than ordinary ones. To identify them, scientists must spy on how they grow, looking for ones that still spread even when an antibiotic drug is around.
For this type of study, scientists usually place bacteria in a liquid growth medium — food, essentially — within a bottle-like flask. Then they jiggle the flask. This makes the bacteria slosh around. Over time, they run into everything in the liquid. Those that adapt to any drugs will eventually grow more quickly, and eventually outnumber all other germs in the flask.
But that flask isn’t much like nature, notes Michael Baym. He is a microbiologist at Harvard Medical School in Boston, Mass. He and his team decided to instead spy on bacteria living on a flat surface. This, after all, would better resemble the sites where bacteria might encounter drugs, such as on hospital counters, door knobs and medical equipment.
On a flat surface, germs ‘see’ only whatever is right next to them, Baym explains. To adapt there, they don’t have to be the best in the whole community. They just have to be survive on whatever real estate is next door.
Microbiologists tend to grow germs in a Petri dish. This is circular, low-walled dish that has a goo rich in nutrients — agar — spread across its bottom. A standard Petri dish is about the size of a human palm. Baym’s team instead created a much larger flat plate. Theirs was a whopping 60 by 120 centimeters (2 by 4 feet) in size. That makes it nearly as large as a foosball table! They called it this plate MEGA, which stands for Microbial Evolution and Growth Arena.
The scientists added one of two common antibiotic drugs to the growth medium spread across the plate: either trimethoprim or ciprofloxacin. But they didn’t add the same amount everywhere. They put small amounts of a drug in the agar that had been spread along the sides of the plates. Then, in bands of agar, they increased the dose of a drug as its distance from the edges increased. They put the highest dose of drug in a band running through the middle. Next, the researchers placed bacteria along the low-dose sides of the plate. These germs were a common version — or strain — of Escherichia coli (Esh-ur-EESH-ee-uh KOH-lye). This germ is best known simply as E. coli.
With the system all set up, the scientists sat back and watched the bacteria grow. The bacteria quickly spred across the bands of agar containing a very low level of a drug. When they reached the edge of the band where the next higher level of poison was located, the cells abruptly stopped spreading. Those that couldn’t live on the higher level of poison either died off or just stopped.
But in a short while, some of the E. coli mutated. That means their genes changed — evolved — in ways that helped them adapt. This let them survive the poison. These strains of the germ now spread into the next band of agar. When they again met a much higher dose of the drug they again stopped. But that didn’t last forever. Before long, some of the bacteria evolved, broke through and began migrating into the next band of agar.
This pattern continued over and over. During some 10 to 12 days, the bacterial colonies spread onward toward the center of the plate. Eventually some arrived at — and colonized — the middle. The drug level there was 1,000 times as high as had been needed to kill some of the initial bacterial pioneers. But eventually, some settlers developed mutations that allowed them to grow even on these strongest dose of poison. Doctors refer to such highly-resistant germs as “superbugs.”
Interestingly, the bacteria that advanced the fastest into the high-drug bands were not always the most super of the superbugs. For some germs, adapting to life with the drugs slowed their growth. This might trap them behind the faster advancing but not as drug-resistant pioneers.
The new findings are important because they can help scientists learn how antibiotic resistance evolves.
Baym and his colleagues think their MEGA-plate could be used to study how bacteria respond to other types of environments also. For example, bacteria may evolve differently when there is not much food available.
His team described its findings in the September 9 issue of Science.







