Some dirt won’t hurt
It could even lower risks of serious allergic disease

A growing number of studies suggest that for everyday hygiene, washing hands with regular soap and water is best. Frequently using soaps or sanitizers with antibacterial chemicals can kill too many germs, which might foster life-threatening allergies.
iStockphoto
Wash your hands!
That familiar piece of advice helps prevent the spread of disease. Good old soap and water remove the bacteria, viruses and other germs that can make you sick. But is there any big advantage to soap laced with bacteria-killing chemicals? Should people sanitize computer keyboards, shopping cart handles and anything else that others have touched?
Indeed, is it possible to be too clean?
Actually, data show, it is. A growing number of studies suggest that routing too many germs might actually foster life-threatening allergies. If you find that hard to believe, it’s probably because you’ve been taught that germs are bad.
Some certainly do trigger serious disease. The word germ probably sets off an alarm in the heads of most people. But the term refers to any microbe. And of the untold numbers of germ species in the world, the vast majority poses little or no harm to most people. Some are even beneficial.
The problem: Antibacterial soaps and sanitizers can’t tell the difference. They are as likely to evict good germs as bad. To stay healthy, then, people need to adopt habits that limit their exposure to bad germs even as they actively welcome others.
Germs are us
Think your body is covered just by skin cells? Think again. Human skin hosts about 10 microbes for every one skin cell. That means your body’s surface is more microbial than human. That same 10-to-1 ratio holds for the digestive tract, the lining of your nose — even the inside of your belly button. Germs are far tinier than human cells. So although microbes have you outnumbered, they still account for only 1 percent to 3 percent of your body’s weight. You share your body with more than 10,000 species of germs. And overall, that’s a good thing.
Without the microbes in your gut, you wouldn’t have any vitamin K. This little-known vitamin plays a vital role in clotting blood when you suffer a cut or nosebleed. Microbes also make B vitamins, which are needed for all kinds of reactions inside your cells. Still other microbes help you digest many nutritious foods.
Even microbes that don’t nourish you play a role in keeping you healthy. They do so by crowding out potential troublemakers. Germs that trigger disease — pathogens — sneak into our bodies all of the time. But if legions of harmless microbes are already there, a disease-causing one won’t find room to multiply enough to make you sick. (That’s the idea behind eating yogurts with “active” cultures, meaning live bacteria.)
Moreover, many microbes educate your immune system. It needs to know which substances in the environment are harmless and which pose a threat. Without that training, the immune system can go into overdrive, triggering dangerous reactions when it shouldn’t.
Wheezing and sneezing
In healthy people, cells of the immune system respond to pathogens and many other foreign substances by attacking them. This is one way our bodies fight infection. Along the way, we may develop a runny nose, cough or other symptoms that mark the body’s attempts to expel the pathogen. Luckily, immune cells in most people recognize harmless microbes as just that: safe. Our immune cells don’t attack them and we stay sniffle-free.
When the immune system fails to learn this lesson, allergies can develop. They signal an overreaction. Now immune cells inappropriately attack things that initially posed no harm, such as pollen or pet dander.
Such allergies can be harmful — even life-threatening. In some people they trigger hives, rashes or itchy skin. In others, asthma — a narrowing of the airways in the lungs — may occur. During an asthma “attack,” people have trouble moving enough air through their breathing passages. Any number of things can launch asthma attacks in susceptible people, including cold air and exercise. Allergies, however, provoke many cases.
The number of people with allergies (including allergic asthma) has been on the rise. But not everywhere. It’s a big problem in North America, Western Europe and other developed nations. Meanwhile, many regions suffering from poor sanitation and hygiene have not seen the same increase. Scientists have been trying to understand what’s behind these surprising trends.
The farm connection
A large drop in the number of people living on small family farms may be one explanation, says Erika von Mutius. She’s a doctor that specializes in childhood allergies at Ludwig Maximilian University in Munich, Germany.

She and her coworkers studied children in rural areas of Germany, Austria and Switzerland. Some lived on farms; others did not. The researchers recorded data about each child’s exposure to farm animals and stables. The experts also looked at whether the child drank unpasteurized milk, as is common on farms. Pasteurization is a heat process designed to kill disease-causing bacteria. Finally the researchers recorded data on asthma and allergy symptoms.
Simply spending time on a farm did not by itself alter allergy risk, they found. But young children who drank unpasteurized milk and spent time in stables were much less likely to develop asthma, hay fever or other allergies later in life. Kids whose mothers had worked in the stables during pregnancy were even better protected than those whose mothers avoided such work.
Von Mutius suspects these findings relate to germs. “The stable is an indicator of microbial exposure,” she says, referring to bacteria and fungi common in such places. Untreated milk also contains microbes. (A word of caution: Raw milk sometimes contains dangerous pathogens. That’s why milk is pasteurized.) Overall, farm microbes appear to offer health benefits. Von Mutius is now probing which microbes are responsible — and why.
Nature’s helping hand
No farm nearby? No problem. Just getting outdoors throughout childhood may lower an individual’s risk of developing allergies, concludes Ilkka Hanski. The ecologist works at the University of Helsinki in Finland. He recently showed that our immune systems are less likely to overreact if we live where many different species abound. Such species richness is known as biodiversity.

His team drew blood from Finnish teens and measured amounts of immunoglobulin E. Levels of this antibody, made by the immune system, soar in people with allergies. The team also sampled microbes living on the kids’ forearms and tallied plant species near their homes.
Their findings proved striking. Teens living in areas with greater plant variety had fewer allergy-linked antibodies in their blood — and a greater diversity of skin microbes. This link was strongest for teens living near forests and farms. However, even having more types of native plants in their yards appeared to be beneficial.
Hanski suspects that contact with nature gives us a chance to pick up microbes that help prevent allergies. “It is likely that some environmental microbes will establish themselves on and in our bodies,” he explains.
Even in mice, research shows, some skin microbes appear to limit allergies. Hanski and his coworkers now think the same holds true for people. Why such germs help remains a mystery. But they might just educate our immune systems.
Hanski suspects these bacteria activate certain cells so that they boost their production of a chemical that calms the immune system. That would reduce the chances of a “wrong” response — and potentially life-threatening reactions.
So where do those beneficial microbes come from? The test bacterium that helped mice normally is found in soil. Others can be found on the surfaces of green plants, according to Tari Haahtela. He is a retired allergy specialist in Helsinki and one of Hanski’s coworkers. Training the immune system with healthy bacteria seems to require little more than getting out into natural areas.
And that’s just what Hanski recommends. Go outdoors and spend as much time as possible in natural environments — somewhat wild areas such as woods and meadows. If there is outdoor space surrounding your home, allow some natural plants to grow there, he says. “Don’t cover it entirely with a lawn and paved areas.” Exposure to a variety of plants — and the microbes they shelter — is particularly important for young children, he says. That’s because the diversity of microbes on their skin is still developing. Once established, those germ communities will tend to remain fairly stable.
Guarding wild germs
A strong immune system depends on exposure to a healthy assortment of microbes. But many of those germs are under assault, says Jeff Lodge. He is a microbiologist at the Rochester Institute of Technology in New York.

Lodge has found that germs in lakes and streams regularly encounter medicines known as antibiotics. These kill bacteria and fungi. Most of these drugs come from wastewater treatment plants. Their source tends to be drugs that people consumed, and then excreted into toilets throughout the nation.
Antibiotics also contaminate the rainwater that runs off of many farms. Here, too, the source is excretion — but from livestock. Sometimes farmers will have given the medicines to sick animals. But more often, they just fed tiny amounts of the drugs to promote the growth of their pigs, chickens and cows.
When antibiotics get into a lake or stream, they kill lots of germs. (The drugs are most effective against bacteria and some fungi. They do nothing against viruses or other pathogens.) Gradually, the surviving germs will adapt, developing genetic changes — mutations — that allow them to live even in the presence of these medicines. Those mutant germs will pass along this resistance to antibiotics as they reproduce. Each new generation will have the same protection against the drug.
So antibiotics in the environment decrease the diversity of microbe species (something Hanski’s study suggests might compromise our health). And any bacteria that survive can become more and more resistant to such medicines.
Lodge has also shown that two widely used antimicrobials — triclosan and triclocarban — are tainting lakes and streams. Manufacturers add these chemicals to hand sanitizers, sponges, dish detergents and other household products. With use, some share of the chemicals wash down the drain. Eventually they can find their way into lakes and streams. And as with antibiotics, bacteria are becoming resistant to them. In fact, some microbes don’t just resist antibacterials — they actually eat the chemicals intended to kill them.
It gets worse. In microbes, a small loop of DNA — called a plasmid — carries the resistance genes for antibiotics and antimicrobials. In the wild, bacteria sometimes swap plasmids. When that happens, Lodge and others find, a germ that’s resistant to antibiotics, antimicrobials or both can pass along that resistance, even to other species. And that can spell really bad news if the newly resistant bacterium is a pathogen.
That’s why Lodge, von Mutius and a number of other scientists recommend avoiding household products labeled as “antibacterial” or “antimicrobial.” Their ingredient list almost always includes triclosan or triclocarban. These chemicals and antibiotics have very useful roles, just not for everyday use in homes and on farms.
Save them for hospitals or where people and animals have already been sickened by bacteria or fungal infections.
And perhaps the simplest prescription: Go out and get dirty. Just be sure to stick to the tried and true when it comes time to wash up. As Lodge points out, “Hot water and plain, ordinary soap can do a great job of cleaning the skin.”
Power Words
allergen A substance that causes an allergic reaction.
antibody A protein made by the immune system that recognizes foreign substances.
antigen A substance capable of causing an immune reaction.
antibiotic A germ-killing substance prescribed as a medicine (or sometimes as a feed additive to promote the growth of livestock).
antimicrobial A substance used to kill or inhibit the growth of microbes. Manufacturers have added some, such as triclosan and triclocarban, to sponges, soaps and other household products.
bacterium (plural bacteria) A single-celled organism forming one of the three domains of life.
germ Any one-celled microorganism, such as a bacterium, fungal species or virus particle. Some cause disease. Others can promote the health of higher-order organisms, including birds and mammals. The health effects of most, however, remain unknown.
hygiene Behaviors and practices that help to maintain health.
immune system The collection of cells and their responses that help the body fight off infection.
dander Flakes of skin in an animal’s fur or hair.
immunoglobulin E One of several types of antibodies made by the immune system.
microbe Short for microorganism.
microorganism An organism that cannot be seen without aid of a microscope.
native plants Types that occur naturally (not because they were planted by people) in a given region.
naturalized Filled with more native types of plants.
pathogen An organism that causes disease.
plasmid A small circular loop of DNA that is separate from the main chromosomal DNA of bacteria.
sanitize The process of removing substances that can spread disease.
virus Tiny infectious agents consisting of RNA or DNA surrounded by protein. Viruses can reproduce only by injecting their genetic material into a host cell.
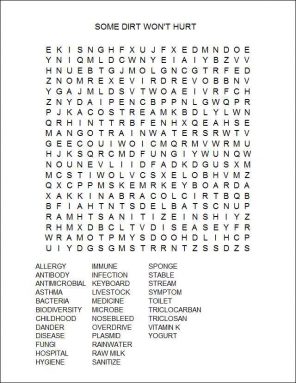
Word Find (click here to enlarge puzzle for printing)