Superbugs: A silent health emergency
Bacteria are outsmarting antibiotics to an alarming degree
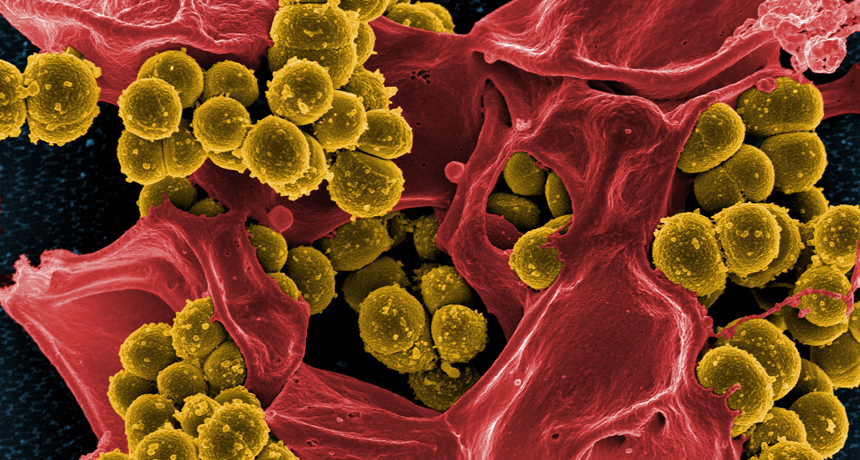
The infamous MRSA “superbug” is shown here (stained in yellow), destroying a person’s white blood cell (red).
National Institutes of Health/Wikimedia Commons
The first of a two-part series.
Bacteria and other microbes can make us sick. But there’s a lurking danger with some germs that’s far more frightening than a bout of food poisoning or an infected wound. Today, drugs exist to fight most of these germs. They’re called antibiotics. Before these medicines came along, common infections frequently killed people. And that’s where the danger lies: What will happen if antibiotics no longer kill germs?
Already some antibiotics have lost their superpowers. Many others are beginning to lose theirs. Biologists describe this problem as resistance. Across the globe, germs are becoming resistant to antibiotic medicines. In a sense, these “superbugs” have begun to laugh at those former wonder drugs.
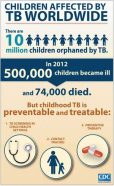
But resistance is no laughing matter. As germs toughen up against drugs that are supposed to slay them, treatable conditions such as TB — tuberculosis — can spread. And surgeries that rely on antibiotics could turn from life-saving to life-threatening.
The threat is huge
“Alarming levels” of drug-resistant bacteria already exist in many parts of the world. That’s the conclusion of a 257-page report published in April. It was issued by the World Health Organization (WHO).
This United Nations agency, based in Geneva, Switzerland, recently reviewed how well these germ slayers perform in 114 countries. In some places, it found, antibiotics no longer work for half of all people being treated against common diseases. Those diseases include pneumonia and gonorrhea.
But even antibiotic-resistant germs that don’t kill can be a problem. Their infections become harder to treat — and more expensive. Consider one estimate — $233 million — published May 20 in the journal Antimicrobial Resistance and Infection Control. That’s how much researchers calculated that it costs the United States each year to deal with just one resistant superbug. That germ causes a lung disease known as pneumonia.
Drug-immune bugs that flourish in the human gut can enter the environment with every flush of the toilet. Researchers discovered how big this problem is when they analyzed wastewater from 11 sites in one French city. Antibiotic-resistant bacteria tainted 96 percent of their samples. A May 1 paper in Clinical Infectious Diseases describes the disturbing details.
Some scientists have scouted for such germs in the environment. They collected superbugs at hospitals. Then they probed the germs, identifying parts of their genes that appear to make them resistant to antibiotics. Next, the researchers looked in the outdoor environment for that same genetic fingerprint of superbugs. And they turned up that superbug DNA in 71 places — from the soil and sea water to human wastes. The researchers reported their findings May 8 in Current Biology.
Why it’s happening
Drug designers have created antibiotics to kill bacteria, as well as some fungi and other germs. But sometimes, a few treated germs survive. They survive because they’re stronger. Or they may have certain genetic mutations that allow them to break down the drug. They might even have evolved a way to keep the drugs from harming their operational machinery. Over time, all germs susceptible to a drug will die off. That will leave behind only superbugs — those microbes that medicines can’t kill.
This is not surprising. In fact, it’s quite natural. Part of evolution, it’s known as survival of the fittest.
Scientists stumbled onto the first antibiotic, penicillin, around 1930. Since then, research has produced a medicine cabinet full of additional ones. It appeared that these would make many of the worst bacterial infections ever more manageable. So, during the 1970s, drug developers began focusing on noninfectious health problems, such as cancer and heart disease. As a result, in the past 30 years, no new types of antibiotics have been developed.
Right now, bacteria are outsmarting antibiotics faster than developers can make new ones. And there are no signs things will change, says Stewart Cole. He directs the Global Health Institute at the Ecole Polytechnique Fédérale de Lausanne in Switzerland.
Writing in the May 12 Philosophical Transactions of the Royal Society B, he argues that the “golden age” of antibiotic development “is a distant memory, and the likelihood of there being another seems slim.” This lack of new types of germ killers, he says, has been allowing superbugs to morph and thrive.

Despite its name, MRSA is resistant to far more antibiotics than just methicillin. That makes this superbug particularly nasty in hospitals and prisons. These are places where people often have open wounds or weak immune systems. Both increase a person’s chance of picking up an infection.
Too much of a good thing
Drug resistance can develop at any time. But its likelihood climbs as the use of an antibiotic increases. And this is especially true when an antibiotic is overused. That’s when a doctor prescribes it for infections it has no hope of curing.
For instance, doctors sometimes prescribe antibiotics to treat an infection before they learn if the disease is caused by bacteria. If viruses are responsible, then antibiotics will be useless. The reason: Antibiotic medicines do not kill viruses. Yet by giving an antibiotic to someone with a viral infection, that drug will reach good bacteria living in our bodies. And over time, some of these bacteria will become resistant to the drug.
Last year, the CDC reported that up to half of the antibiotics that U.S. doctors prescribed went to people who didn’t actually need them.
Take, for example, someone who visits a doctor for a lingering cough. Viral infections cause most coughs. So a viral cough won’t be helped by drugs and will tend to go away on its own. Yet 71 percent of the time, doctors will still prescribe antibiotics for patients coming in with a common cough, a May 21 study finds.

A small number of people who visit a doctor with a cough turn out to have bacterial pneumonia. These cases do require antibiotic treatment. But Linder says doctors should easily be able to recognize these few from the hordes of people coming in with a routine, viral cough.
Perilous profit
Antibiotic overuse also has become a problem on farms. In the United States, animals — not people — receive about 80 percent of all antibiotics. Sometimes the drugs are used to save an infected animal or prevent disease from spreading through a herd. More often, though, feed suppliers put small amounts of these drugs into the food that will be given to healthy animals. These antibiotics help speed the animals’ growth. And this has boosted farmers’ profits.
But using antibiotics just to beef up livestock is “a direct threat to human health,” argues Kellogg Schwab. He’s an environmental microbiologist at Johns Hopkins University in Baltimore, Md. Earlier, he and his coworkers detected bacteria that are resistant to antibiotics in the exhaust air blowing out of farm buildings. That suggests these superbugs can spread through the air from animals to people.

Germs that are immune to antibiotics also can hitch a ride into your body through ground beef or the chicken breast on your cutting board. Biologists have found that much of the fresh beef, pork and poultry sold in grocery stores contains bacteria resistant to antibiotics.
Even if those germs don’t sicken us or cause other immediate harm, they can offload their resistance genes into other bacteria that normally live inside our bodies. Sometimes, like with the MRSA superbug, resistance is carried on circular pieces of DNA called plasmids. These plasmids can slip easily from one bacterial cell into another.
In this way, our gut microbes can become “a reservoir of resistance,” says Sharon Peacock. She’s a microbiologist at the University of Cambridge in England. Later, “when we actually get sick and need an antibiotic, we may already carry a resistance gene” that may keep that drug from working, she says.
In the United States, farmers have fought against banning antibiotics as growth promoters. They say it will reduce their profits because more animals will get sick, slowing their growth. But that’s not been the experience in other countries.
The U.S. Food and Drug Administration, or FDA, has proposed banning antibiotic use in healthy animals. But for more than 30 years, the livestock industry and Congress have fought such action. Recently, the FDA stepped up its efforts to end this practice.
In December 2013, FDA laid out a plan to phase out within three years the use of antibiotics on farms to boost livestock growth. Its stated reason: concern that farm use of these drugs has made more germs immune to the antibiotics needed to fight life-threatening infections in people. And that’s a worry because the same germs that sicken animals often sicken people.
Antibiotic resistance is a complex and growing problem. Many microbiologists worry that the time when antibacterial medicines no longer work could be coming. Thankfully, doctors and many patients are becoming more aware of the problem. Researchers also are hard at work creating new tools to keep superbugs from taking over.
Next: How scientists are trying to tackle the problem
Power Words
antibiotic A germ-killing substance prescribed as a medicine (or sometimes as a feed additive to promote the growth of livestock). It does not work against viruses.
bacterium (plural bacteria) A single-celled organism forming one of the three domains of life. These dwell nearly everywhere on Earth, from the bottom of the sea to inside animals.
boils (in medicine) A skin infection that starts as a hard, red, painful lump. Eventually, it gets bigger, softens and fills with pus. A common source of these is a bacterium known as Staphylococcus aureus.
bioengineer A researcher who applies technology for the beneficial manipulation of living things. Bioengineers use the principles of biology and the techniques of engineering to design organisms or products that can mimic, replace or augment the chemical or physical processes present in existing organisms. This field includes researchers who genetically modify organisms, including microbes. It also includes researchers who design medical devices such as artificial hearts and artificial limbs.
Centers for Disease Control and Prevention, or CDC An agency of the U.S. Department of Health and Human Services, CDC is charged with protecting public health and safety by working to control and prevent disease, injury and disabilities. It does this by investigating disease outbreaks, tracking exposures by Americans to infections and toxic chemicals, and regularly surveying diet and other habits among a representative cross-section of all Americans.
cholera A bacterial disease that infects the small intestine, causing sever diarrhea, vomiting and dehydration. It is spread by germs from feces that contaminate water or food.
DNA (short for deoxyribonucleic acid) A long, spiral-shaped molecule inside most living cells that carries genetic instructions. In all living things, from plants and animals to microbes, these instructions tell cells which molecules to make.
evolution A process by which species undergo changes over time, usually through genetic variation and natural selection, that leave a new type of organism better suited for its environment than the earlier type. The newer type is not necessarily more “advanced,” just better adapted to the conditions in which it developed.
fungus (plural: fungi) Any of a group of unicellular or multicellular, spore-producing organisms that feed on organic matter, both living and decaying. Molds, yeast and mushrooms are all types of fungi.
gene A segment of DNA that codes, or holds instructions, for producing a protein. Offspring inherit genes from their parents. Genes influence how an organism looks and behaves.
germ Any one-celled microorganism, such as a bacterium, fungal species or virus particle. Some germs cause disease. Others can promote the health of higher-order organisms, including birds and mammals. The health effects of most germs, however, remain unknown.
gonorrhea A serious disease that can infect the genitals, rectum and throat. This sexually transmitted disease is very common, especially among people between the ages of 15 and 24. Untreated, it can cause infertility or death. “Untreated gonorrhea may also increase your chances of getting or giving HIV – the virus that causes AIDS,” according to the U.S. Centers for Disease Control and Prevention.
growth promoter (in livestock agriculture) A medicine, usually an antibiotic, added in small doses to the feed given to animals raised for meat. Used as a preventive medicine, it can reduce the risk that animals will become sick, which would slow their growth. And that would decrease a farmer’s profits.
immune system The collection of cells and their responses that help the body fight off infection.
infection A disease that can be transmitted between organisms.
influenza (or flu) A highly contagious viral infection of the respiratory passages causing fever and severe aching. It often occurs as an epidemic.
livestock Animals raised for meat or dairy products, including cattle, sheep, goats, pigs, chickens and geese.
microbe Short formicroorganism. A living thing that is too small to see with the unaided eye, including bacteria, some fungi and many other organisms such as amoebas. Most consist of a single cell.
microbiology The study of microorganisms, principally bacteria, fungi and viruses. Scientists who study microbes and the infections they can cause or ways that they can interact with their environment are known as microbiologists.
mutation Some change that occurs to a gene in an organism’s DNA. Some mutations occur naturally. Others can be triggered by outside factors, such as pollution, radiation, medicines or something in the diet. A gene with this change is referred to as a mutant.
plasmid A small circular loop of DNA that is separate from the main chromosomal DNA of bacteria.
pneumonia A lung disease in which infection by a virus or bacterium causes inflammation and tissue damage. Sometimes the lungs fill with fluid or mucus. Symptoms include fever, chills, cough and trouble breathing.
resistance (as in drug resistance) The reduction in the effectiveness of a drug to cure a disease, usually a microbial infection. (as in disease resistance) The ability of an organism to fight off disease.
superbug A popular term for a disease-causing germ that can withstand medicines.
toxic shock syndrome A rare and potentially deadly bacterial infection caused by Staphylococcus aureus. This bacterium release toxins — natural poisons — into the body of its host. Symptoms include a sudden high fever, muscle aches, vomiting, diarrhea, a rash and sometimes seizures.
toxin A poison produced by living organisms, such as germs, bees, spiders, poison ivy and snakes.
tuberculosis A bacterial disease that causes unusual growths in the lungs or other tissues. Untreated, it can kill. The infection usually spreads when a sick individual coughs (or talks, sings or sneezes), spewing germs into the air.
virus Tiny infectious particles consisting of RNA or DNA surrounded by protein. Viruses can reproduce only by injecting their genetic material into the cells of living creatures. Although scientists frequently refer to viruses as live or dead, in fact no virus is truly alive. It doesn’t eat like animals do, or make its own food the way plants do. It must hijack the cellular machinery of a living cell in order to survive.
World Health Organization An agency of the United Nations, established in 1948, to promote health and to control communicable diseases. It is based in Geneva, Switzerland. The United Nations relies on the WHO for providing international leadership on global health matters. This organization also helps shape the research agenda for health issues and sets standards for pollutants and other things that could pose a risk to health. WHO also regularly reviews data to set policies for maintaining health and a healthy environment.