Use of injectable GLP-1 weight-loss drugs skyrockets among teens
Such drugs and other hunger-suppressing tech raise questions about long-term use and safety

Injectable GLP-1 drugs are not for kids looking to shed a few pounds in the short term. They’re intended to help reduce excess weight to improve health — with the understanding that people may regain that weight as soon as they stop taking the medication.
SDI productions/E+/Getty Images Plus
Share this:
- Share via email (Opens in new window) Email
- Click to share on Facebook (Opens in new window) Facebook
- Click to share on X (Opens in new window) X
- Click to share on Pinterest (Opens in new window) Pinterest
- Click to share on Reddit (Opens in new window) Reddit
- Share to Google Classroom (Opens in new window) Google Classroom
- Click to print (Opens in new window) Print
About one in five U.S. kids have obesity. This condition greatly ups their risk of heart disease, type 2 diabetes, stroke and more. Such dangers partially explain doctors’ interest in helping people avoid excessive weight. Lately, many kids and teens have been turning to a new class of injectable drugs to help them reduce weight. And soon they may have another option, too: a mechanical pill to suppress appetite.
Questions remain, however, about the safety of such weight-loss tactics, especially for young people.
Obesity is a complex problem and can have many root causes. They may include poor diet, too little exercise and high levels of stress. Genetics and some health conditions can also play a role.
“I’m just very concerned about how we’re using these medications as a quick fix for a complex problem,” says Dan Cooper. A pediatrician, he works at the University of California, Irvine.
Do you have a science question? We can help!
Submit your question here, and we might answer it an upcoming issue of Science News Explores
Lauren Oshman, though, resists calling these drugs a “quick fix.” A family doctor, she teaches at the University of Michigan in Chelsea. More than a decade ago, the American Medical Association declared obesity a disease. But some people, Oshman says, seem to feel certain medical conditions “are okay to treat with drugs and others are not.”
Take, for instance, ADHD (short for attention deficit/hyperactivity disorder). Doctors regularly treat it with drugs, she notes. “Would we say that Adderall [for ADHD] is a quick fix?”
A bigger issue, Cooper says, is the long-term safety of what’s being prescribed to manage weight today — both in kids and adults. Right now, reliable long-term data do not exist. The new treatments are just that: too new.
Widespread use in young people
In 2021, the U.S. Food and Drug Administration, or FDA, approved a new class of drugs for weight loss. They’re known as GLP-1s. (That stands for glucagon-like peptide-1 receptor agonists.) Most people know them by their trade names, such as Wegovy and Ozempic.
Initially, such drugs were approved solely to manage diabetes. After the FDA’s 2021 ruling for weight loss, however, their use skyrocketed. That was true especially among young people. Some GLP-1s are approved for kids as young as 12.
From 2020 to 2023, prescriptions for these injectables in adolescents and young adults jumped nearly six-fold — by 594 percent. That’s according to a June 2024 study in the Journal of the American Medical Association.
Oshman was part of the team that used data from U.S. pharmacies to tally how often GLP-1 drugs are now being prescribed to children and teens. The rapid trend to prescribe them to adolescents surprised her.
Their use also skyrocketed among women aged 18 to 25 — by 659 percent. In men that age, the increase was not quite as high — 481 percent.
GLP-1s fool the hunger meter
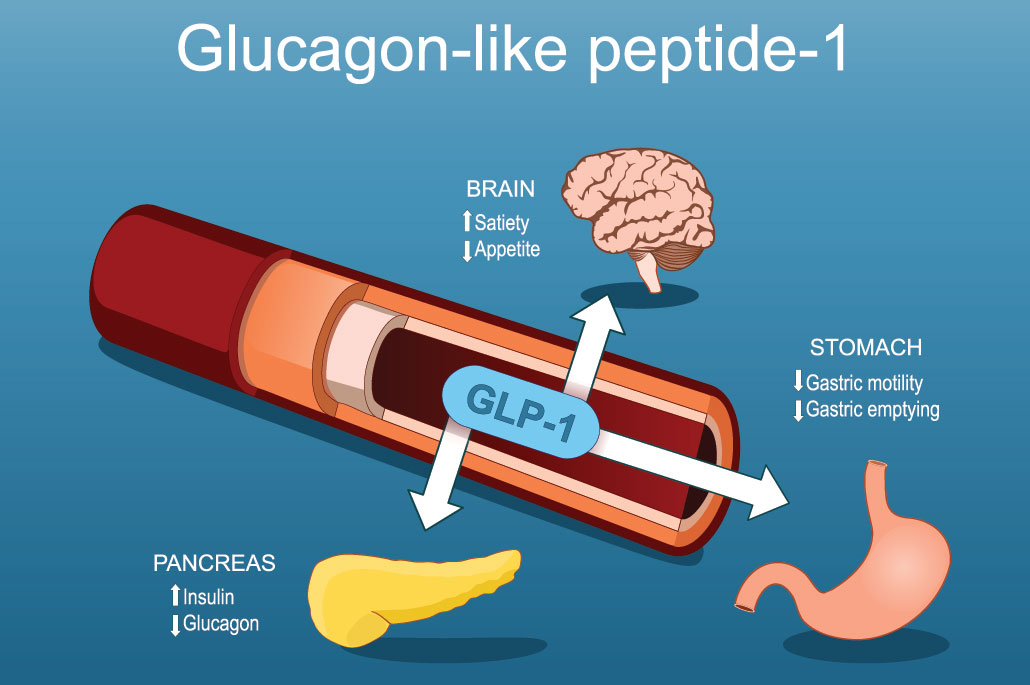
These drugs work by mimicking the action of GLP-1. It’s a hormone the gut makes to announce that food is coming and will soon be broken down into the sugar that will feed cells throughout the body.
GLP-1 triggers a series of important actions. It tells the pancreas to make insulin. That’s a hormone that will later move food-derived sugar into cells. GLP-1 also reduces levels of glucagon, another hormone; that one increases levels of sugar in the blood. And in the stomach, GLP-1 delays the emptying of food.
The result: GLP-1 drugs trick our hunger meters so people now feel full longer on less food. Without the drive to eat as much, most people lose weight.
But doctors are divided about how much they should be prescribed for obesity in kids.
“There’s a lot of controversy amongst pediatricians, pediatric endocrinologists and physicians in general about how we should be treating pediatric obesity,” says Oshman. After all, the drug isn’t recommended for short-term use. In fact, once people stop taking these drugs, their appetite — and weight — will likely come back.
At issue: Many overweight kids experience stigma over their weight. And that may drive a host of other health problems, including mental-health ones. For these kids, many families and doctors may judge that GLP-1 drugs may be worth taking, at least in the absence of known risks.
Good VIBES
Researchers at the Massachusetts Institute of Technology, in Cambridge, have taken a different approach to reducing our urge to overeat. The robotic pill they’ve created is called VIBES (for vibrating ingestible bioelectronic stimulator). Once swallowed, this motorized pill tricks the stomach into thinking it’s full.
A little motor in each pill makes it wiggle. When taken before a meal, that action turns on receptors that sense how much the stomach is stretching. Normally, that stretching comes from the arrival of food, Shriya Srinivasan explains. So the pills make you feel fuller than you actually are. She calls it “a whole new way” to manage weight.

Srinivasan is a bioengineer who led the VIBES study while working at MIT. (Today she works at nearby Harvard University.) “We’re kind of piggybacking on a natural mechanism in the body,” she says.
You’d swallow the pill about a half hour before eating, she says. Acid in the stomach will then dissolve a coating on the pill. This releases a tiny spring-loaded pin, which turns on a motor. At once, the pill begins to shake.
Some 40 minutes later, it stops. Then, it passes through the body and out in your poop. The team has tested it in pigs. In early studies, the pigs ate about 40 percent less in a meal. Srinivasan’s team shared its findings in the December 2023 Science Advances.
The MIT team chose 80 hertz — or 80 shakes per second — as the optimal frequency for the pills’ vibrations. Any faster and people could hear them buzz inside the pigs!
Tricking the body into feeling full
Neuroscientist Tim Moran wasn’t involved in the VIBES study. But his lab at the Johns Hopkins School of Medicine, in Baltimore, Md., studies how the brain and gut communicate to decide that you’re full. While eating, he notes, “you’ve got signals arising from both the intestine and the stomach.” They’re announcing the arrival of food. Those signals come from multiple types of receptors. Some look for chemical evidence of a meal. Others check for physical signs, such as stomach stretching.
The VIBES pill attempts to trigger those stretch receptors, he says. It’s trying to “fool the system that the stomach is full when it’s actually not.”

Vibrating pills might be novel. But VIBES works similarly to another device, Moran says. He points to intragastric balloons, or IGBs. As the name suggests, these are balloons that partially fill your stomach to trigger those stretch receptors.
Hans-Rudolf Berthoud is skeptical about such attempts to “trick the body.” This type of approach, he thinks, “is a little bit naïve.” By that, he means it may ignore things that could keep it from working as well as expected.
A neurobiologist, Berthoud works at Louisiana State University in Baton Rouge. His concerns come from past findings with IGBs: Over time, they stop working. After about 10 to 12 weeks, people begin eating the old amount of food again. Berthoud predicts something similar will happen with VIBES. The researchers “present all kinds of results [that are] interesting,” he says. “But I think it will just end just like the balloons.”
Those balloons also had many risks. Some burst inside the stomach. Others got stuck in the digestive tract. Such complications could turn deadly. After the FDA issued warnings on IGBs, some companies stopped selling them.
Future studies will look at such risks for VIBES, says Srinivasan. The pills, which are big, are in early trials. One pill measures almost 40 millimeters (1.6 inches) long and is a fourth as wide.
The pig studies did not give any signs that the pills will harm the stomach. Still, VIBES is a long way from being available for doctors to prescribe. And if it is, there will also be the question of what happens when the pills get pooped out into the environment. For now, Srinivasan says, the materials that make up its battery should pose little harm to living things.
A new era of weight management
Innovations such as VIBES, combined with the rapid spread of GLP-1 drugs, point to how desperately people want weight-loss solutions.
These two new approaches work somewhat differently. VIBES works primarily in the stomach. GLP-1s “work predominantly in the brain,” says Cooper at UC Irvine. And as for those drugs, they really work, he says. “When you talk to people who are taking these drugs, they repeatedly say, ‘you know, I just don’t think about eating anymore.'”
That explains why Cooper’s not surprised by the rapid uptick in GLP-1 prescriptions reported by Oshman’s group. Pediatricians see a lot of kids struggling with obesity, he says. And those pediatricians are worried. They want to do something to help.
“I’m not at all criticizing that,” Cooper says. However, many questions remain regarding the long-term use and safety of such drugs.
Future studies should answer such questions. And those answers will help doctors to prescribe this powerful class of medicines responsibly.







