Therapeutic robots may soon swim within the body
Scientists look to nature for clues about how to build and power these microrobots
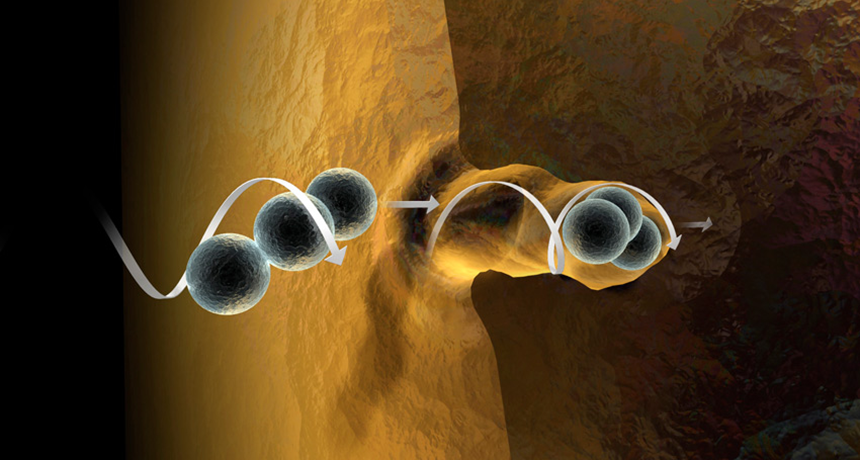
A computer model shows a robot called a microswimmer boring through plaque, a fatty material that can build up inside someone’s arteries. Too much plaque can block the arteries and lead to a heart attack. These microrobots are barely visible to the human eye — they’re about the size of a speck of dust.
Min Jun Kim
Imagine a microscopic machine that could swim through a person’s blood vessels on its way to delivering medicine to a cancerous tumor. Or one that unclogs an artery to prevent a heart attack, or even performs delicate vision-saving surgery from inside the eye. These feats aren’t possible yet. But researchers are designing miniature robots, called microswimmers, that may soon do all of these things. And more.
Imagine a robot and Star Wars’ beloved R2-D2 may come to mind, or his pal C-3PO. The robots scientists want to deploy in the human body are much, much smaller. They’re typically less than 1 millimeter (0.04 inch) in size. At their largest, they might be the size of a few grains of table salt. But they can be much smaller — so small that they can be seen only with a microscope.
The human body is made up mostly of wet stuff. Blood, spinal fluid and other liquids make up about 60 to 65 percent of the volume of the human body. So to move through this environment with ease, robots must swim. But finding the right materials and designs to send robots swimming through even the tiniest blood vessels has proven tough. But not impossible. Indeed, scientists have been inching toward this vision throughout the past decade.
The payoff should be worth the wait, says David Cappilleri. He’s a microroboticist at Purdue University in West Lafayette, Ind. “Microrobots can go places that larger robots can’t.” What’s more, he argues, “they can handle tools with finer precision.”
Humans don’t have much experience moving things around micro-environments of the body, explains Bradley Nelson. He’s a roboticist at the Swiss Federal Institute of Technology in Zurich. But some other organisms do this well. So Nelson and other robot designers are looking to them for inspiration.
Copying nature’s microswimmers
Before scientists could create robots to swim inside the body, they first had to solve the problem of scale. The physics of swimming changes as an object gets smaller and smaller, Nelson observes. That’s because on a microscopic scale, liquids become much more viscous. (Viscosity is the thickness of a liquid.)
“If you were to shrink down to the size of a [microrobot] and jump into a pool of water,” says Nelson, “the water wouldn’t feel like water anymore. It would feel like thick honey.”
That’s why he and other scientists have copied some of nature’s tiniest swimmers: single-celled lifeforms that infect people. These master swimmers can navigate swiftly through our bodies.
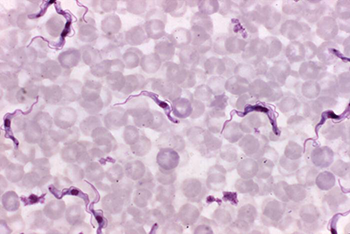
For design tips, Nelson focused on a type of microbe known as a protozoan. He picked the species Trypanosoma brucei (Try-PAN-oh-SO-mah BRU-see-eye). In people, this parasite causes African sleeping sickness. Affected people often can’t sleep at night but are overcome with drowsiness by day.
T. brucei swims through the bloodstream by swishing a whiplike tail. This tail is called a flagellum (Fla-JEL-um).
As it moves, T. brucei also changes its shape. This helps it get from one part of the body to another. The protozoan can go from short and stumpy to slender and needle-like. That lets it penetrate blood vessel walls and invade the spinal cord.
Nelson liked the idea of building a microrobot with this talent for shape-shifting. Such a robot could do jobs in different parts of the body, depending on its shape. These tasks might include unclogging arteries or delivering medicines, Nelson explains. Or maybe the robot could make microscopic repairs in the blood vessels of the eye.
He used a gel-like material to build a soft microrobot. By altering the gel’s temperature, he can make his robot short and stumpy or long and needle-like.
Nelson described this new design last year in the journal Nature Communications.
Putting tiny robots to work inside the body

Nelson’s soft-bodied microswimmer isn’t the only nano-medic that researchers are building. Some at Drexel University in Philadelphia, Penn., created a different type to bring cancer-killing medicine to tumors.
One challenge to designing robots that will go inside the body is powering them. These robots are too small to carry an engine or battery pack, notes Min Jun Kim, who led the Drexel team.
Kim is a mechanical engineer. (He now works at Southern Methodist University in Dallas, Texas.) Mechanical engineers use rules of motion, energy and force to design and build machinery. Kim’s team used magnets to solve the power problem. Unlike Nelson’s soft microswimmer, Kim’s design is made entirely of metal.
He looked to bacteria for inspiration. And he found it in Borrelia burgdorferi (Bor-REL-ee-ah Burg-DOR-fur-eye). This spiral-shaped germ causes an illness known as Lyme disease. People fall ill after being bitten by an infected tick. The bacterium uses a corkscrew-like motion to swim and bore through tissue.
Kim mimicked its corkscrew shape by joining together strands of magnetic beads. Those beads are so small they can barely be seen without a microscope.
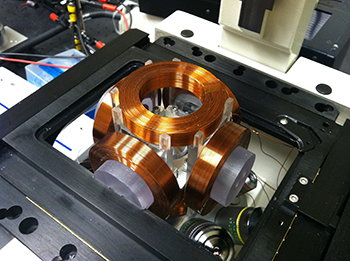
He used magnets to propel his microrobot through artificial blood vessels in a petri dish. By increasing or decreasing the strength of the magnets, Kim can make the robot swim faster or slower. Changing the direction of the magnetic field lets him steer the robot left or right. He can join several chains together to make strands as long as 20 to 30 beads. Or he can break them apart into strands as short as three beads.
Kim says the surfaces of these beads could be coated with medicines. To treat cancer, a microswimmer that’s a longer chain could bore into a thick tumor. Once inside, it could break apart into smaller chains to spread its cancer-killing medicine around, he says.
Kim’s team shared its findings last year in the journal Scientific Reports.
Challenges remain
Some microrobots can already swim in petri dishes. But there would likely be big hurdles before they could be released in people, notes Zhang Li. He studies nanotechnology — the design and harnessing of extremely small devices — at the Chinese University of Hong Kong. Scientists need to know, for instance, how safe the itty-bitty devices are. They also need to know how to remove those tiny swimmers once their work is done, Li notes.
For now, researchers plan to test their microscopic devices in animals such as mice. Those tests can also help scientists make sure that the materials in their robots aren’t toxic.
Scientists also can use animals to practice inserting, tracking and removing microswimmers before they put them in people. Working with robots in a real body — whether a human or a mouse — is a lot different than doing it in a petri dish under a microscope, Li explains. In a petri dish, there’s no skin, blood or other tissues to block the view.
Despite these challenges, scientists find this “an exciting time” Li observes. “There’s so much left to learn.”