Tiny spongelike machines sop up blood sugar
In mice, microscopic devices patrol the bloodstream to treat diabetes

Some people with diabetes must give themselves shots of medication every day. The injections contain a hormone called insulin. This keeps their blood sugar level from rising too high. But researchers are inventing shot-free ways to control diabetes.
AndreyPopov/istockphoto
In a laboratory in China, a horde of miniscule, bloblike machines flow in a mouse’s blood. The tiny machines, or nanomachines, are a brand-new invention. They could completely change the way people treat a disease called diabetes.
Diabetes disrupts the body’s ability to control the level of sugar in the blood. If blood sugar gets too high or too low, a person (or mouse) could get sick or even die.
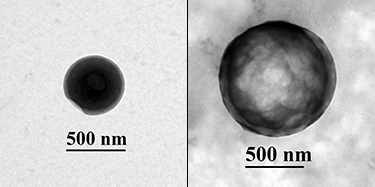
These nanomachines are working to prevent that. They patrol the blood, seeking sugar. Each machine is a hollow, plastic ball just one one-hundredth the diameter of a human hair. When a lot of sugar is in the blood, the nanomachine sops it up and swells in size. When the blood sugar level is low, sugar seeps out of the ball.
Chemist Jianzhong Du of Tongji University in Shanghai, China, invented this nanomachine. He calls it a “sugar sponge.”
In healthy people (or mice), the body maintains a consistent level of sugar in the blood on its own. This sugar comes from food. After digestion, sugar travels through the bloodstream, providing fuel the body needs.
The body’s cells feast on a form of sugar called glucose. They need a steady supply of the stuff in order to do their jobs. Since people don’t eat constantly, the body must store some sugar for later. The liver plays an important role in this process. It tucks away extra sugar, releasing it gradually as the body needs it. The liver can also make sugar itself.
But the liver needs a way to know how much sugar is in the blood already. Hormones help with this. These chemicals are like keys that unlock certain liver cells. Depending on which kind of key arrives, the liver will either make or stash more sugar. Insulin is a hormone that signals the liver to store sugar.
Tiny ‘sponges’ sop up and squeeze out sugar
In people with diabetes, the body either doesn’t make any insulin or doesn’t use it correctly. Without insulin, the whole system gets out of whack. The level of glucose in the blood can get dangerously high or low. People with diabetes must carefully track the level of sugar in their blood. Some must also give themselves shots of insulin. Sometimes, they need to do this several times a day. Ouch! Other times, they may forget a shot or take too much insulin. A mistake like this could make a person very sick.
Du wondered if a new approach might improve the lives of people with diabetes. Maybe he could help them avoid pesky insulin shots. He decided to develop a nanomachine that could absorb and release sugar. “The natural function of the liver inspired me to develop this new technique,” he says.
The sugar sponge is essentially a hollow, plastic sphere. But its surface also contains a special protein called concanavalin A. This protein sticks to glucose, trapping it within the sphere. Du says, “Like sponges sop up water and swell, our sugar sponge absorbs glucose and swells.” The process works in reverse, too. A soaking wet sponge on a dry surface leaks slowly. Similarly, when the amount of glucose in the blood stream is low, the sugar sponge can’t hold onto all its sugar. It will release it slowly.
Du’s team tested the sugar sponge in mice. The team started with a group of 20 diabetic mice. Five mice received a sugar sponge injection. The rest got injections with similar materials that didn’t absorb sugar. Only the sugar sponge made a difference. It brought the level of sugar in the mice’s blood into a normal range. The benefit lasted for two days. After that, the diabetic mice once again had too much sugar in their blood.
Du and his colleagues reported their results in the Journal of the American Chemical Society in May.
The invention is not yet ready for people to use. “There is still a long way to go,” says Du. His team is working to increase the amount of time that the effect lasts. “We are aiming for [the treatment] to last one week, one month or even longer,” he says. Getting a sugar sponge injection every month would certainly be more convenient than insulin shots every day.
Omid Veiseh, who was not involved in the research, thinks the concept of the sugar sponge is imaginative and creative. However, he worries about the fact that the sugar sponges contain concanavalin A. This protein could trigger an allergic reaction, he says.
To better understand how the treatment might affect humans, Du says, his team must take several steps. First, they must test the sugar sponge on animals that are more similar to humans, such as macaque monkeys. They also need to make sure that the proteins and plastics in the sugar sponge won’t damage organs such as the kidney and liver.
A shield for new insulin-making cells
Veiseh is trying a different approach to help diabetics avoid insulin injections. He is a bioengineer at Rice University in Houston, Texas. A bioengineer is a scientist who builds tools to solve medical problems.
Some people develop diabetes because their own immune systems attack and destroy the cells that make insulin. Veiseh and his colleagues have found a way to replace these cells. They start with stem cells. These are seedlike cells that can develop into any type of cell in the body. Genes provide the instructions that tell stem cells what to grow into. Veiseh’s team used specific genes to prompt human stem cells to grow into insulin-making cells.
But just placing these new cells into the body of a person with diabetes wouldn’t help. The person’s immune system would attack and destroy them. The cells needed a shield. The researchers decided to use a gel called alginate, which originally comes from brown algae. They tested 800 variations of this gel in experiments with mice and primates. One worked better than all the others to protect the cells from an immune system attack.
“We call it a protective bubble,” says Veiseh. In a follow-up experiment, his team implanted shielded cells into mice with diabetes. The cells helped the mice produce their own insulin again. His team reported their results in the March 2016 issue of Nature Medicine.
Miniature protective bubbles and tiny sugar-seeking spheres both sound like something out of a science fiction story. But both are real. Thanks to innovators like Du and Veiseh, the field of medicine is getting more and more high-tech every day.
This is one in a series presenting news on technology and innovation, made possible with generous support from the Lemelson Foundation.







