Sore knees may get 3-D printed relief
The printers could sculpt new cartilage or produce devices to deliver drugs

Teen researchers are developing 3-D printing techniques to repair damaged cartilage and other tissues.
busracavus/iStockphoto
By Sid Perkins
PITTSBURGH, Pa. — When it comes to building replacement body parts, 3-D printed plastics have proven their worth. Doctors have printed prosthetic fingers and hands, for instance, to replace ones that their patients had lost in accidents. Veterinarians have printed replacement legs and feet for injured pets. But the latest wave in 3-D printing for medicine goes beyond a reliance on long-lived plastic. Two award-winning examples got their national debut here, two weeks ago, at a major science competition.
This year’s Intel International Science & Engineering Fair brought together almost 1,800 finalists from 81 nations, regions and territories. The students competed for about $5 million in prizes and scholarships. Two of them worked on the cutting edge of medicine to design new 3-D printed implants.
Anna Feldbush, 19, built a tissue-like replacement for damaged cartilage in knees and other joints. A 12th grader, she attends West Shore Junior/Senior High School in Melbourne, Fla. Bhargav Ramesh, 16, developed a new way to support damaged tissues as they heal. He is an 11th grader at duPont Manual High School in Louisville, Ky.
About one in every three finalists took home some award. Anna’s project earned a second-place in materials science. That’s a field of research that analyzes the properties of materials or designs new materials with specific traits. Intel Foundation provided the award, worth $1,500. Bhargav snagged a second-place award, worth $500, from the Samvid Educational Foundation.
Tweaking a printer
Knees are joints that really take a beating. Fortunately, cartilage cushions bones that come together at joints. It keeps bones from rubbing together painfully. But wear and tear can damage that cartilage. This tissue is slow to heal, Anna notes, largely because it doesn’t have its own blood supply. So athletes and many others can end up losing that beneficial joint-cushioning tissue. The result can be intense pain — and sometimes a need for surgery to replace the joint.
Anna wanted to 3-D print some replacement cartilage.

Most 3-D printers, she notes, melt some type of plastic. They slowly dispense this so-called “ink” through tiny nozzles. A computer controls the back-and-forth movement of those nozzles. As the plastic cools, it hardens into some computer-designed solid. But Anna wasn’t interested in printing plastic. She wanted her printer to squeeze out a material that was more like natural cartilage.
The recipe for her ink included a gelatin. It’s a protein that readily dissolves in water. She added a chemical called sodium alginate (AL-jih-nayt) and then mixed both into a solution that also included calcium chloride. That last chemical, over time, helps the gelatin chemically bond to the sodium alginate. This bonding, Anna explains, helps create a firm solid.
Anna had to develop a new printer design to handle her novel ink. She started with an off-the-shelf 3-D printer. Then, she swapped out some parts. These included the system that pumped her solution through the printer. She also replaced the printer’s nozzles with tiny needles. Doctors often use similar-size needles to take blood samples or to give injections.
Anna tested a lot of recipes for her ink. She wanted the end product to be as similar to real cartilage as possible. And as a materials scientist, she tested six properties of each mock-cartilage, including how slick and squishy it was. Anna now estimates that her best ink recipe should cost less than a penny to print enough cartilage to repair a damaged knee. And because the printer works so quickly, she says a new joint cushion could be printed right in an operating room during joint-replacement surgery.
This artificial cartilage might last about 10 years, Anna says. That’s about how long the parts used in a total knee replacement typically last. What’s more, she suspects that her approach to knee repair might well be easier and less painful.
Multipurpose printing
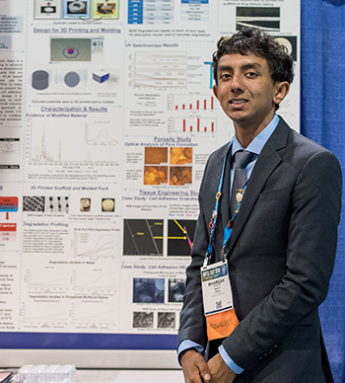
Sometimes doctors aren’t looking to make materials to permanently replace a body’s tissues. Instead, they’re looking to create something that aids healing, then dissolves when it’s no longer needed. That’s what Bhargav investigated.
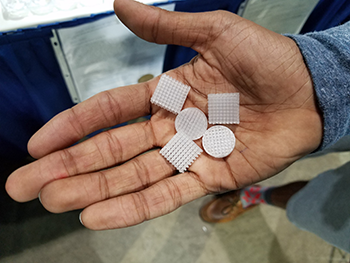
He wanted to print what doctors call a scaffold. Such structures support tissues as they heal or regrow. Scaffolds tend to be porous. That allows cells to move into them, latch on and then grow, the teen explains. Some scaffolds are permanent. He wanted to create one that was temporary and would dissolve, leaving behind only living tissue.
Bhargav’s recipe included just two ingredients. One was polyethylene glycol (Pah-lee-ETH-uh-leen GLY-kol), or PEG. It’s a polymer that biodegrades. That means it will break down in the body over time. The other component was polylactic acid, or PLA. It, too, is a polymer that naturally degrades. These materials firm up to provide a strong material to which cells can attach. But over time they will down and will be flushed from the body.
Like Anna, Bhargav tested different recipes to see which worked best.
A 50:50 blend of PEG and PLA hardened into a brittle — and easily breakable — solid. But both a 3:1 and 9:1 mix of PLA to PEG worked well for scaffolding. In Bhargav’s tests, two types of cells quickly latched onto and then grew upon his fibrous polymer scaffolds. Those tests also showed that the polymers would have dissolved after spending somewhere between 5 and 8 weeks in the body. That’s more than enough time for most tissues to heal, the teen explains.
Each polymer that Bhargav used costs about $80 per kilogram (or about $36 per pound). That might sound like a lot. But porous scaffoldings have so much empty space inside them that they can be made using very little material. Plus, many of them are small to begin with. Together, this means that some types of scaffolding might be 3-D-printed for just a few dollars each.
These materials could serve as more than scaffolding, adds Bhargav. They might deliver drugs. As a material dissolves away, any medicine embedded in it would be gradually released into the body. So, the teen tested this, too. And he showed that the embedded drug he used was released in amounts big enough to be effective.
Society for Science & the Public created ISEF and has been running the competition since 1950. (The Society also runs Science News for Students and this blog.) Intel sponsored this year’s event.
Follow Eureka! Lab on Twitter







